Acute pancreatitis poses a formidable challenge in critical care medicine. Effective fluid management is pivotal in treating this condition. This comprehensive analysis explores fluid therapy intricacies for patients with pancreatic inflammation, providing insights into optimal resuscitation strategies.
Grasping acute pancreatitis pathophysiology is essential for implementing appropriate fluid resuscitation techniques. The inflammatory cascade often leads to severe hypovolemia, necessitating prompt, tailored fluid therapy. This guide equips healthcare professionals with knowledge to navigate complex clinical scenarios.
Evidence-based approaches to fluid management in acute pancreatitis encompass initial assessment and ongoing monitoring. Various aspects, including fluid types, administration timing, and potential complications, are scrutinized. Mastering these principles can significantly improve patient outcomes and mitigate severe complication risks.
Key Takeaways
- Prompt fluid resuscitation is vital in acute pancreatitis management
- Understanding pancreatic inflammation helps guide fluid therapy decisions
- Careful assessment of fluid status is crucial for effective treatment
- Different fluid types may be used based on individual patient needs
- Monitoring fluid responsiveness helps prevent complications
- Tailored approaches are necessary for special patient populations
Understanding Acute Pancreatitis Pathophysiology
Acute pancreatitis manifests as a complex inflammatory condition of the pancreas. This inflammation initiates a cascade of events, potentially leading to severe complications without proper treatment. The intricate pathophysiology demands comprehensive understanding for optimal management.
Inflammatory Response and Fluid Loss
Pancreatic tissue damage in acute pancreatitis triggers the release of inflammatory mediators. These substances induce capillary leak syndrome, causing fluid shifts from intravascular spaces to surrounding tissues. Consequently, substantial fluid loss occurs, compromising hemodynamic stability.
Third-Space Fluid Sequestration
Fluid accumulation in the third space—regions outside intravascular and intracellular compartments—is a hallmark of acute pancreatitis. This sequestration exacerbates intravascular volume depletion, further destabilizing the patient’s hemodynamic status. The resultant fluid imbalance necessitates prompt intervention.
Impact on Cardiovascular System
Massive fluid shifts and the inflammatory cascade in acute pancreatitis can precipitate hypovolemic shock. This state of inadequate tissue perfusion may trigger systemic inflammatory response syndrome (SIRS). SIRS poses a significant risk of multi-organ dysfunction, underscoring the gravity of acute pancreatitis.
| Pathophysiological Process | Effect | Potential Complication |
|---|---|---|
| Pancreatic inflammation | Release of inflammatory mediators | Capillary leak syndrome |
| Capillary leak syndrome | Fluid loss from intravascular space | Third-space fluid sequestration |
| Third-space fluid sequestration | Intravascular volume depletion | Hypovolemic shock |
| Hypovolemic shock | Inadequate tissue perfusion | Systemic inflammatory response syndrome (SIRS) |
Mastery of these pathophysiological processes is paramount for effective fluid management in acute pancreatitis. Prompt intervention can attenuate the inflammatory cascade’s progression and avert severe complications. Clinicians must remain vigilant, employing evidence-based strategies to optimize patient outcomes.
Early Recognition and Assessment of Fluid Status
Rapid identification of fluid status is vital in managing acute pancreatitis. Clinicians initially assess vital signs, skin turgor, and urine output. These markers provide crucial insights into a patient’s fluid equilibrium, guiding immediate interventions.
Laboratory indicators are essential for evaluating fluid status. Hematocrit and blood urea nitrogen (BUN) serve as critical markers. Elevated levels typically indicate dehydration and significant fluid depletion, necessitating prompt action.
Hemodynamic parameters offer profound insights into fluid balance. Blood pressure, heart rate, and central venous pressure inform fluid resuscitation strategies. These measurements enable clinicians to assess the efficacy of fluid therapy and make necessary adjustments.
| Parameter | Normal Range | Implications in Acute Pancreatitis |
|---|---|---|
| Hematocrit | 35-45% | Elevated: Indicates hemoconcentration due to fluid loss |
| BUN | 7-20 mg/dL | Increased: Suggests dehydration and renal dysfunction |
| Urine Output | 0.5-1 mL/kg/hr | Decreased: Indicates poor renal perfusion and fluid deficit |
Swift intervention based on comprehensive assessments is paramount. It mitigates potential complications and informs initial fluid resuscitation protocols. Continuous monitoring of these parameters ensures optimal fluid management throughout the treatment course, enhancing patient outcomes.
Fluid Management in Acute Pancreatitis: Core Principles
Optimal fluid management is pivotal in acute pancreatitis treatment. Mastering fundamental principles enables clinicians to deliver superior care and enhance patient outcomes significantly.
Initial Resuscitation Goals
Goal-directed therapy underpins fluid management in acute pancreatitis. The primary objective is restoring intravascular volume and maintaining tissue perfusion. Aggressive early fluid resuscitation is critical to avert complications and organ dysfunction.
Timing of Fluid Administration
The initial 24-48 hours are pivotal for fluid management. Swift fluid administration during this phase counteracts fluid losses and mitigates pancreatic necrosis risk. Vigilant monitoring of fluid responsiveness is imperative to guide ongoing therapeutic interventions.
Choice of Resuscitation Fluids
Selecting appropriate fluids is paramount for effective treatment. Balanced crystalloids are superior to normal saline, offering lower chloride content and reduced metabolic acidosis risk. Key considerations include:
- Use of lactated Ringer’s solution or Plasma-Lyte
- Avoiding excessive chloride administration
- Monitoring electrolyte balance
Adherence to these core principles optimizes fluid management in acute pancreatitis. This approach potentially mitigates complications and substantially improves patient outcomes, enhancing overall treatment efficacy.
Types of Fluids Used in Pancreatitis Treatment
Fluid management is essential in acute pancreatitis treatment. Various fluids restore electrolyte balance and maintain tissue perfusion. This analysis examines the primary fluid categories utilized in pancreatitis care.
Crystalloid Solutions
Crystalloid solutions are the primary choice for initial resuscitation. Normal saline and Ringer’s lactate stand out as popular options. Normal saline, widely accessible and economical, may induce hyperchloremic acidosis in large quantities.
Ringer’s lactate, a balanced solution, closely resembles the body’s electrolyte composition. Its formulation aims to minimize potential electrolyte imbalances associated with high-volume fluid administration.
Colloid Solutions
Colloid solutions contain larger molecules, providing prolonged intravascular presence. Albumin and hydroxyethyl starch exemplify this category. While offering rapid volume expansion, their application in pancreatitis remains contentious due to potential adverse effects and increased costs.
Balanced vs Unbalanced Solutions
Balanced solutions, such as Ringer’s lactate, are formulated to maintain electrolyte equilibrium more effectively than unbalanced alternatives like normal saline. Their composition mirrors plasma electrolyte proportions, potentially mitigating acid-base disturbances.
| Fluid Type | Examples | Advantages | Disadvantages |
|---|---|---|---|
| Crystalloids | Normal saline, Ringer’s lactate | Cost-effective, widely available | May cause electrolyte imbalances in large volumes |
| Colloids | Albumin, Hydroxyethyl starch | Rapid volume expansion | Higher cost, potential side effects |
| Balanced Solutions | Ringer’s lactate | Better electrolyte balance | May not be suitable for all patients |
Monitoring Fluid Responsiveness
Acute pancreatitis necessitates meticulous fluid management through vigilant monitoring of fluid responsiveness. Clinicians employ diverse methodologies to evaluate patient reactions to fluid therapy. These approaches encompass both static and dynamic parameters, each offering distinct insights into a patient’s fluid status.
Central venous pressure (CVP) exemplifies static parameters. Despite its historical utilization, CVP exhibits limitations in accurately predicting fluid responsiveness. Dynamic parameters, conversely, furnish more dependable information regarding a patient’s fluid equilibrium.
Pulse pressure variation (PPV) and stroke volume variation (SVV) represent crucial dynamic parameters. These measurements elucidate blood flow fluctuations throughout respiratory cycles. Such data provides invaluable insights into a patient’s fluid responsiveness, facilitating more precise therapeutic interventions.
| Parameter | Type | Reliability | Limitations |
|---|---|---|---|
| Central Venous Pressure | Static | Low | Affected by various factors |
| Pulse Pressure Variation | Dynamic | High | Requires mechanical ventilation |
| Stroke Volume Variation | Dynamic | High | Affected by cardiac arrhythmias |
Continuous monitoring of these parameters enables clinicians to optimize fluid therapy with precision. By meticulously tracking PPV and SVV fluctuations, healthcare providers can judiciously adjust fluid administration. This approach mitigates potential complications and enhances patient outcomes in acute pancreatitis cases.
Complications of Inadequate Fluid Management
Inadequate fluid management in acute pancreatitis precipitates severe complications, exacerbating patient outcomes and prolonging hospitalizations. Recognizing these risks is paramount for implementing efficacious treatment strategies and mitigating potentially life-threatening sequelae.
Organ Dysfunction
Suboptimal fluid balance frequently engenders organ dysfunction, with the kidneys exhibiting particular susceptibility. Acute kidney injury, a prevalent complication, may necessitate dialysis and protract recovery periods. This renal impairment can significantly impact overall patient prognosis and management.
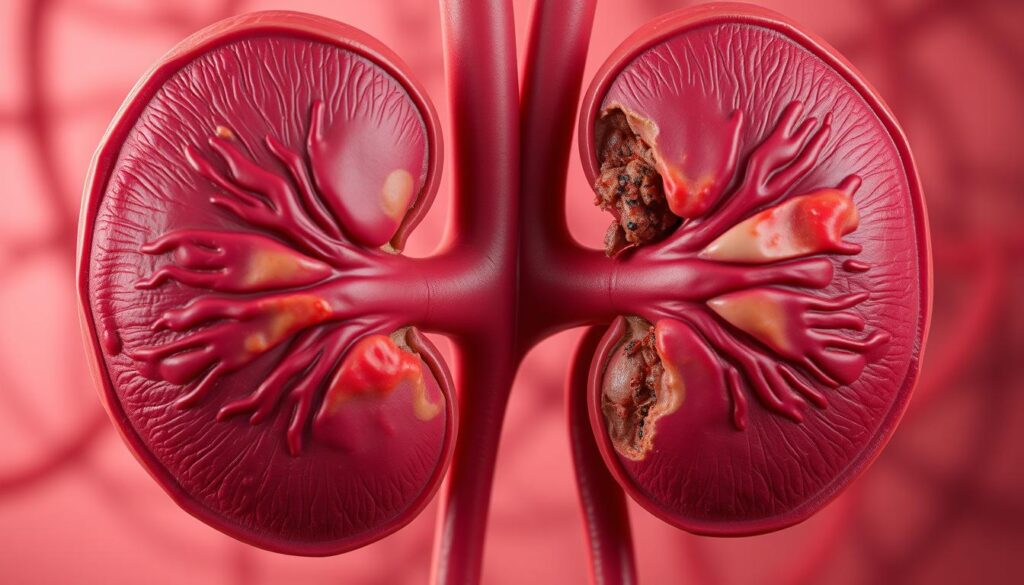
Pancreatic Necrosis
Insufficient fluid resuscitation can induce pancreatic tissue necrosis, amplifying infection risk and potentially mandating surgical intervention. Judicious fluid therapy maintains pancreatic perfusion, mitigating necrosis risk. This preservation of pancreatic viability is crucial for averting long-term complications and ensuring optimal recovery.
Systemic Complications
Inadequate fluid administration may precipitate a cascade of systemic perturbations. Persistent Systemic Inflammatory Response Syndrome (SIRS) can evolve, culminating in multi-organ failure. Abdominal compartment syndrome, another grave complication, engenders elevated intra-abdominal pressure and organ compression.
- Cardiovascular instability
- Respiratory distress
- Metabolic imbalances
Vigilant monitoring of fluid status and dynamic therapy adjustments are imperative for complication prevention. Expeditious recognition coupled with prompt intervention is fundamental for optimizing patient outcomes in acute pancreatitis. These proactive measures can significantly reduce morbidity and mortality associated with this critical condition.
Advanced Hemodynamic Monitoring Techniques
Advanced hemodynamic monitoring is indispensable in managing complex acute pancreatitis cases. These sophisticated techniques guide fluid therapy and optimize cardiovascular function in critically ill patients, enhancing their chances of survival.
Transpulmonary thermodilution emerges as a pivotal method in hemodynamic monitoring. This technique measures cardiac output and extravascular lung water, offering crucial insights into a patient’s fluid status. It involves injecting cold saline into a central vein and measuring temperature changes in the femoral artery.
Echocardiography provides real-time visualization of cardiac function, assessing ventricular filling, contractility, and valvular function. Clinicians can employ either transthoracic or transesophageal approaches, depending on the specific clinical scenario and required level of detail.
Pulse contour analysis estimates cardiac output by analyzing the arterial pressure waveform. This less invasive method offers continuous monitoring but may necessitate frequent recalibration in unstable patients to maintain accuracy.
Noninvasive cardiac output monitoring techniques have gained traction in recent years. These include bioimpedance and bioreactance methods, which measure changes in thoracic electrical properties to estimate stroke volume and cardiac output.
| Technique | Invasiveness | Continuous Monitoring | Key Parameters |
|---|---|---|---|
| Transpulmonary thermodilution | Invasive | Yes | Cardiac output, Extravascular lung water |
| Echocardiography | Minimally invasive | No | Cardiac function, Valvular status |
| Pulse contour analysis | Minimally invasive | Yes | Cardiac output, Stroke volume variation |
| Noninvasive cardiac output monitoring | Non-invasive | Yes | Cardiac output, Stroke volume |
Each hemodynamic monitoring technique possesses unique strengths and limitations. The selection of an appropriate method hinges on the patient’s condition, available resources, and specific clinical questions. Integrating multiple monitoring modalities often yields the most comprehensive assessment of hemodynamic status in acute pancreatitis patients.
Special Considerations in Fluid Management
Fluid management in acute pancreatitis demands a personalized strategy, particularly for patients with intricate medical conditions. Geriatric medicine principles, heart failure complications, and chronic kidney disease significantly influence treatment approaches. These factors necessitate meticulous consideration when devising fluid management protocols.
Elderly Patients
Geriatric patients often exhibit diminished physiological reserves and multiple comorbidities. Prudent fluid administration is imperative to avert fluid overload in this demographic. Vigilant observation for volume overload indicators, such as peripheral edema or respiratory distress, is paramount.
Cardiac Compromise
Heart failure patients encounter distinctive challenges in fluid management. Striking a balance between adequate tissue perfusion and pulmonary edema risk necessitates rigorous monitoring. Echocardiography and biomarkers like BNP can effectively guide fluid therapy in these complex scenarios.
Renal Dysfunction
Chronic kidney disease exacerbates fluid balance complexities in acute pancreatitis. These patients may exhibit limited capacity to excrete excess fluid, heightening the risk of fluid overload. Severe cases might necessitate continuous renal replacement therapy to maintain optimal fluid balance.
| Condition | Fluid Management Considerations | Monitoring Parameters |
|---|---|---|
| Elderly Patients | Slow infusion rates, frequent reassessment | Urine output, skin turgor, mental status |
| Heart Failure | Cautious fluid administration, diuretic use | Jugular venous pressure, lung auscultation |
| Chronic Kidney Disease | Restricted fluid volumes, electrolyte balance | Serum creatinine, potassium levels, fluid balance |
Complex cases demand a tailored approach to fluid management. Consistent reevaluation and modification of fluid therapy based on patient response are essential. This strategy ensures optimal outcomes while minimizing potential complications associated with fluid imbalances.
Role of Nutrition in Fluid Management
Nutrition is pivotal in managing fluid balance for acute pancreatitis patients. The timing and type of nutritional support significantly influence patient outcomes and recovery trajectories. Optimal nutritional strategies can mitigate complications and expedite healing processes.
Enteral Nutrition Timing
Early enteral feeding is the preferred approach in acute pancreatitis management. This method preserves gut barrier function and minimizes potential complications. Research demonstrates that initiating enteral nutrition within 48 hours of admission correlates with reduced infection rates and shortened hospital stays.
Impact on Fluid Balance
Effective nutrition management is crucial in controlling fluid retention. Enteral feeding supports metabolic requirements while minimizing the risk of fluid overload. Conversely, parenteral nutrition may exacerbate excessive fluid accumulation, potentially compromising patient recovery.
| Nutrition Type | Impact on Fluid Balance | Effect on Gut Function |
|---|---|---|
| Early Enteral Feeding | Helps maintain balance | Preserves gut barrier function |
| Delayed Enteral Feeding | May lead to fluid retention | Potential gut barrier dysfunction |
| Parenteral Nutrition | Higher risk of fluid overload | Possible gut atrophy |
Achieving equilibrium between nutritional requirements and fluid management is paramount for optimal metabolic support. Clinicians must vigilantly monitor patients’ responses to feeding interventions. Continuous assessment and strategy adjustments are essential to prevent complications and facilitate recovery.
Evidence-Based Protocols and Guidelines
Clinical practice guidelines are paramount in managing acute pancreatitis. The American College of Gastroenterology and International Association of Pancreatology have issued comprehensive fluid management recommendations. These protocols aim to standardize treatment approaches and improve patient outcomes.
Early aggressive fluid resuscitation is a cornerstone of these guidelines. Goal-directed resuscitation protocols are advocated to tailor fluid therapy to individual patient needs. This approach allows for precise fluid administration based on specific physiological parameters.
The American College of Gastroenterology recommends lactated Ringer’s solution for initial fluid resuscitation. The suggested rate is 250-500 mL per hour, adjusted according to patient response and risk factors. This regimen aims to restore intravascular volume and maintain organ perfusion.
| Organization | Recommended Fluid | Initial Rate | Monitoring Parameters |
|---|---|---|---|
| American College of Gastroenterology | Lactated Ringer’s solution | 250-500 mL/hr | Urine output, BUN, hematocrit |
| International Association of Pancreatology | Balanced crystalloids | 5-10 mL/kg/hr | MAP, heart rate, CVP |
Conversely, the International Association of Pancreatology advocates for balanced crystalloids at 5-10 mL/kg/hr. They emphasize monitoring mean arterial pressure, heart rate, and central venous pressure. These parameters guide fluid therapy adjustments and ensure optimal tissue perfusion.
Adherence to these evidence-based protocols can mitigate complications and enhance patient care. By implementing these guidelines, clinicians can optimize fluid management strategies. This approach ultimately leads to improved outcomes in acute pancreatitis patients.
Prevention and Management of Fluid Overload
Fluid overload poses a significant risk in acute pancreatitis treatment. Effective recognition and management are crucial for preventing complications and optimizing patient outcomes. Clinicians must remain vigilant to ensure proper fluid balance throughout the treatment process.
Recognition of Fluid Overload
Identifying fluid overload requires attention to specific indicators. Weight gain, edema, and pulmonary edema serve as primary signs. Daily fluid balance monitoring enables early detection of potential issues.
Healthcare professionals should be alert to increased respiratory rates and decreased oxygen saturation. Crackles detected during lung auscultation may also indicate fluid accumulation. These symptoms necessitate immediate intervention to prevent further complications.
Correction Strategies
When fluid overload is identified, prompt action is necessary. Strategies include:
- Fluid restriction to limit further volume accumulation
- Administration of diuretics to promote fluid elimination
- Ultrafiltration for severe cases unresponsive to diuretics
Monitoring Parameters
Close monitoring is vital during fluid overload correction. Key parameters include:
| Parameter | Target Range | Frequency |
|---|---|---|
| Urine Output | 0.5-1 mL/kg/hr | Hourly |
| Central Venous Pressure | 8-12 mmHg | Every 2-4 hours |
| Serum Electrolytes | Within normal limits | Daily |
| Body Weight | Stable or decreasing | Daily |
Effective fluid overload management in acute pancreatitis requires diligent implementation of corrective strategies. Continuous monitoring of key parameters enables timely adjustments to treatment protocols. This approach significantly reduces complication risks and enhances overall patient outcomes.
Conclusion
Effective fluid management is paramount in acute pancreatitis treatment. A tailored approach, meticulously adapted to each patient’s unique requirements, is imperative for optimal outcomes. This strategy necessitates a delicate equilibrium between fluid resuscitation, vigilant monitoring, and judicious adjustments based on individual physiological responses.
A multidisciplinary collaboration, encompassing intensivists, gastroenterologists, and nursing personnel, is fundamental to successful management. This synergistic effort facilitates comprehensive care and expeditious reactions to fluctuations in patient status. Consistent reevaluation and modification of fluid therapy protocols are indispensable components of this methodology.
Continuous research in acute pancreatitis fluid management refines our comprehension and enhances treatment protocols. These advancements concentrate on optimizing fluid types, administration timing, and volume to augment patient outcomes. Healthcare providers must remain abreast of emerging evidence and adapt their clinical practices accordingly.
By implementing evidence-based strategies and maintaining a patient-centric focus, clinicians can markedly improve acute pancreatitis outcomes. The future of pancreatitis management hinges on ongoing education, rigorous research, and the application of sophisticated, personalized fluid management techniques.