Esophageal dysphagia, a complex disorder, impairs the esophagus’s function, hindering the passage of food from the mouth to the stomach. This condition profoundly impacts an individual’s quality of life, potentially leading to severe health complications if not addressed1.
In the United States, approximately one in 25 adults encounter a swallowing problem annually, underscoring the widespread nature of this issue2. Distinguished from oropharyngeal dysphagia, which affects the mouth and throat, esophageal dysphagia is characterized by a sensation of food being lodged in the chest or throat.
Esophageal dysphagia can stem from a variety of causes, including muscular disorders, neurological conditions, and structural anomalies within the esophagus. Common etiologies include achalasia, esophageal spasm, tumors, gastroesophageal reflux disease (GERD), and scleroderma12.
Dysphagia can manifest at any age but is notably prevalent among the elderly. This heightened risk is attributed to aging, esophageal wear and tear, and conditions such as stroke or Parkinson’s disease1. Grasping the causes, symptoms, and treatment modalities for esophageal dysphagia is imperative for effective management and enhanced patient outcomes.
Key Takeaways
- Esophageal dysphagia affects the esophagus, causing difficulty swallowing
- It’s more common in older adults but can occur at any age
- Various medical conditions can cause esophageal dysphagia
- Symptoms include food getting stuck in the chest or throat
- Early diagnosis and treatment are crucial to prevent complications
- Multiple treatment options are available, depending on the cause
- Lifestyle changes can help manage symptoms in some cases
Understanding Esophageal Dysphagia
Esophageal dysphagia, a complex disorder, affects the esophagus, the muscular conduit between the throat and stomach. It impairs the normal swallowing mechanism and esophageal function, resulting in a myriad of symptoms that profoundly affect an individual’s quality of life.
Definition and Basic Concepts
Dysphagia is perceived as a subjective difficulty or abnormality in swallowing3. Esophageal dysphagia manifests post-swallow initiation, primarily within the esophagus. It differs from oropharyngeal dysphagia, which involves challenges in initiating a swallow and potential nasopharyngeal regurgitation3.
How Normal Swallowing Works
The swallowing process is a complex interplay of muscle and nerve coordination in the mouth, throat, and esophagus. When functioning optimally, these components facilitate the movement of food and liquids from the mouth to the stomach. Any disruption in this process can precipitate dysphagia symptoms, including difficulty initiating a swallow or the sensation of food being stuck in the throat.
Impact on Quality of Life
Esophageal dysphagia can profoundly impact an individual’s quality of life. It may lead to malnutrition, weight loss, and dehydration4. In severe instances, dysphagia can result in choking, potentially life-threatening if food becomes lodged in the throat4. These challenges often precipitate social isolation due to difficulties with eating and drinking, further exacerbating overall well-being.
“Understanding the basic concepts of esophageal function and the swallowing process is crucial for recognizing and addressing dysphagia symptoms effectively.”
Early recognition of esophageal dysphagia symptoms can facilitate timely intervention and improved outcomes. Various treatment modalities exist, including esophageal dilation, surgical interventions for conditions such as esophageal tumors, and prescription medications for dysphagia caused by GERD4.
Types of Swallowing Disorders
Swallowing disorders, medically termed as dysphagia, afflict millions within the United States. Approximately 10 million individuals are impacted, with prevalence escalating to about 15% among adults aged 50 and above5. These afflictions are broadly categorized into oropharyngeal dysphagia and esophageal dysphagia.
Oropharyngeal dysphagia pertains to challenges in initiating the swallowing process within the mouth and throat. Conversely, esophageal dysphagia, constituting roughly 70% of all dysphagia cases, impacts the esophagus, hindering the passage of food and liquids to the stomach5.
Swallowing difficulties arise from diverse etiologies. Neurological conditions, such as Parkinson’s disease, stroke, or amyotrophic lateral sclerosis (ALS), account for approximately 37% of dysphagia cases5. Additional factors include:
- Brain or nerve disorders such as multiple sclerosis
- Nerve damage from spinal cord injuries
- Esophageal issues like abnormal tissue growth or muscle spasms
- Gastroesophageal reflux disease (GERD) and acid reflux, accounting for about 12% of cases56
Accurate symptom recognition is paramount. Approximately 70% of patients with dysphagia experience coughing, gagging, or choking during swallowing5. Additional indicators may encompass chest pain, a sensation of food being lodged in the throat, regurgitation, and challenges in consuming solids or liquids6.
Proper diagnosis and treatment are essential for managing swallowing disorders. Diagnostic methodologies encompass upper endoscopy, barium swallow studies, and esophageal manometry6. Treatment modalities are tailored to the underlying cause, spanning from dietary adjustments to surgical interventions.
Common Causes and Risk Factors
Grasping the etiology of dysphagia is paramount for efficacious management and treatment. A myriad of medical conditions, neurological disorders, and structural anomalies contribute to the causes of swallowing disorders.
Medical Conditions
Chronic acid reflux emerges as a primary offender in esophageal dysphagia, accounting for approximately 75% of esophageal strictures and being the most prevalent cause of chronic esophagitis7. Gastroesophageal reflux disease (GERD) significantly elevates the risk of developing strictures and reflux esophagitis87.
Neurological Disorders
Neurological afflictions such as multiple sclerosis, Parkinson’s disease, and stroke can impede swallowing function. These conditions often disrupt muscle control and coordination, precipitating dysphagia.
Structural Problems
Structural anomalies within the esophagus can physically impede swallowing. Esophageal cancer, strictures, and injuries from caustic ingestion or thermal damage are prevalent culprits7. Untreated esophagitis can precipitate scarring, narrowing, and even Barrett’s esophagus, thereby increasing the risk of esophageal cancer8.
Age-Related Factors
Age significantly influences the risk of dysphagia. Older adults are more susceptible to swallowing difficulties due to muscle atrophy and the increased prevalence of related conditions. The act of taking medication while lying down or right before sleep, coupled with advancing age, are risk factors for medicine-induced esophagitis8.
Other risk factors for dysphagia include specific medications, radiation therapy to the neck or chest, and frequent use of over-the-counter pain relievers7. A history of allergic reactions such as asthma, atopic dermatitis, and allergic rhinitis can also elevate the risk of eosinophilic esophagitis8.
Recognizing the Warning Signs
Esophageal dysphagia manifests through a spectrum of physical symptoms and complications. Identifying these signs of swallowing difficulty at an early stage is imperative to avert severe health consequences and to ensure timely medical intervention.
Physical Symptoms
Common indicators of dysphagia include the sensation of food lodging in the throat or chest, pain during swallowing, and regurgitation. Patients may also experience coughing, gagging, or hoarseness during meals. Difficulty in swallowing, food impaction, chest pain, heartburn, and vomiting are typical manifestations of eosinophilic esophagitis (EoE), a prevalent cause of dysphagia9.
Associated Complications
Esophageal dysphagia can precipitate severe complications such as choking hazards, aspiration pneumonia, malnutrition, and dehydration. In children, EoE may lead to failure to thrive9. Chronic acid reflux, a common etiology of dysphagia, can escalate to Barrett’s esophagus or even esophageal cancer in severe instances10.
When to Seek Medical Help
It is essential to consult a healthcare provider if swallowing difficulties persist or intensify. Immediate medical attention is warranted for unexplained weight loss, chest pain, or difficulty breathing. Prompt diagnosis through upper endoscopy with biopsy and allergy testing can identify underlying conditions like EoE9. For dysphagia caused by chronic acid reflux, a healthcare professional can recommend appropriate treatments, including medications, lifestyle modifications, or surgical interventions if deemed necessary10.
“Early recognition of dysphagia symptoms is key to preventing severe complications and improving quality of life.”
Diagnostic Procedures and Tests
Accurate dysphagia diagnosis necessitates a multifaceted strategy. Initially, a detailed medical history and physical examination are conducted. Subsequently, specialized evaluations are employed to identify the root cause of swallowing impediments.
Swallowing assessments frequently commence with a barium swallow study. This method leverages X-rays to delineate the esophagus’s anatomy during the act of swallowing. It is instrumental in detecting structural anomalies or aberrant muscular activity.
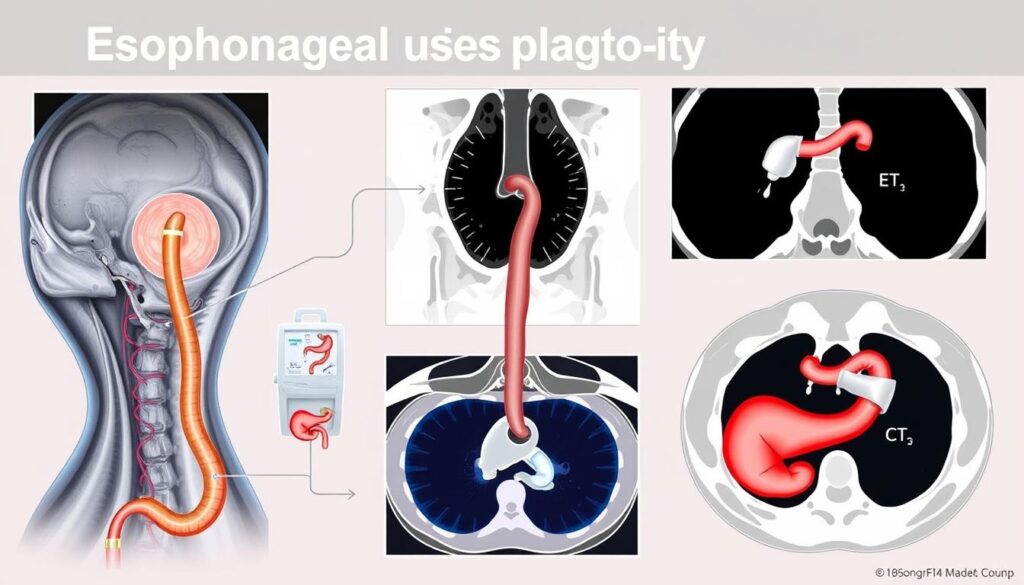
Endoscopy emerges as a pivotal tool in esophageal diagnostics. A slender, flexible tube, equipped with a camera, enables direct visualization of the esophagus’s interior. This modality is critical for uncovering inflammation, tumors, or other pathologies that may precipitate dysphagia.
Manometry, a subsequent evaluation, quantifies the esophageal muscles’ pressure and coordination. This test is indispensable for diagnosing motility disorders. Occasionally, CT or MRI scans are employed to evaluate for tumors or structural anomalies.
The selection of diagnostic modalities is contingent upon the patient’s symptoms and the suspected underlying pathology. Dysphagia diagnosis is paramount, given its prevalence among various patient populations. For instance, 66.67% of stroke patients necessitate swallowing rehabilitation, and 35% to 45% of Parkinson’s disease patients develop swallowing dysfunction11.
| Diagnostic Test | Purpose | Procedure |
|---|---|---|
| Barium Swallow | Visualize esophagus during swallowing | Patient swallows barium liquid while X-rays are taken |
| Endoscopy | Direct visualization of esophagus | Camera-equipped tube inserted through mouth |
| Manometry | Measure esophageal muscle pressure | Pressure-sensitive catheter inserted through nose |
| CT/MRI Scan | Assess for tumors or structural issues | Non-invasive imaging of chest and neck area |
Timely and precise diagnosis is imperative, as dysphagia can lead to severe complications. For example, the incidence of pneumonia in stroke patients with oropharyngeal dysphagia is approximately 25% over a six-month period11. Adequate esophageal testing is crucial for averting such outcomes and guiding efficacious treatment strategies.
Medical Imaging and Evaluation Methods
Esophageal imaging and swallowing tests are indispensable in diagnosing and evaluating dysphagia. These methodologies offer profound insights into the esophagus’s structure and function. Such knowledge is crucial for healthcare providers to devise targeted treatment plans.
Barium Swallow Studies
Barium swallow studies are a pivotal diagnostic tool for esophageal dysphagia. Patients ingest a barium-containing liquid, which enhances visibility on X-rays. This procedure can unveil structural anomalies, narrowing, or irregular esophageal movements12. For oropharyngeal dysphagia, a modified barium swallow is frequently the preferred diagnostic method13.
Endoscopic Examinations
Upper endoscopy is a critical method for dysphagia evaluation. It entails the insertion of a flexible tube with a camera into the esophagus, enabling direct visualization of internal structures. This technique is particularly effective in identifying conditions such as esophageal strictures, tumors, or eosinophilic esophagitis13.
Manometry Testing
Esophageal manometry assesses the pressure and coordination of esophageal muscles. This test is essential for diagnosing motility disorders, such as achalasia. It provides invaluable information regarding the function of the lower esophageal sphincter and esophageal contractions.
| Evaluation Method | Primary Use | Key Information Provided |
|---|---|---|
| Barium Swallow | Esophageal Dysphagia | Structural abnormalities, narrowing |
| Modified Barium Swallow | Oropharyngeal Dysphagia | Swallowing process visualization |
| Upper Endoscopy | Esophageal Dysphagia | Direct visualization, tissue sampling |
| Manometry | Motility Disorders | Muscle pressure and coordination |
In certain instances, additional imaging techniques are employed. For example, ultrasound is useful for evaluating palpable neck masses that might be causing dysphagia13. The selection of evaluation method is contingent upon the suspected cause and location of the swallowing difficulty, ensuring a comprehensive dysphagia evaluation.
Treatment Approaches and Options
Esophageal dysphagia treatment is contingent upon the underlying etiology. At specialized clinics, such as Johns Hopkins Dysphagia and Deglutition Clinic, patients receive bespoke care for a spectrum of conditions, from the natural aging process to neurological disorders14.
Medical Interventions
Physicians may prescribe medications to mitigate acid reflux or relax the esophageal muscles. In instances of infection-induced swallowing difficulties, antibiotics are employed. Mayo Clinic, celebrated for its digestive disorder treatment, annually treats over 16,000 patients with swallowing issues15.
Surgical Solutions
In severe cases, surgical interventions are deemed necessary. Procedures such as laparoscopic Heller myotomy for achalasia or stent placement for esophageal narrowing are employed. Esophageal dilation, a procedure to stretch and expand constricted areas, is frequently conducted at specialized clinics14.
Therapeutic Techniques
Swallowing therapy is a pivotal aspect of dysphagia treatment. Speech language pathologists, such as Rina Abrams at Johns Hopkins, employ behavioral and strengthening techniques to enhance swallowing function14. These exercises focus on improving muscle coordination between the mouth, tongue, throat, and esophagus.
For comprehensive care, institutions like Mayo Clinic offer multidisciplinary approaches. Their top-ranked digestive disorder departments in Rochester, Phoenix/Scottsdale, and Jacksonville provide advanced diagnostic and treatment options for both adults and children with swallowing difficulties15.
Lifestyle Modifications and Management
Effective management of esophageal dysphagia necessitates profound lifestyle adjustments. A bespoke dysphagia diet is pivotal in mitigating discomfort and averting complications. Patients are often required to adopt a regimen of smaller, more frequent meals, accompanied by the meticulous cutting of food into diminutive pieces to facilitate effortless swallowing16.
Employing specific swallowing techniques can markedly enhance the safety and efficacy of the eating process. Techniques such as the chin tuck or head turn are employed to redirect food away from the airway. Additionally, maintaining proper posture during meals is imperative for ensuring safe swallowing.
Adapting one’s eating habits is fundamental to dysphagia management. Patients are frequently counseled to consume food at a slower pace, ensuring thorough mastication, and to eschew foods with textures or temperatures that exacerbate symptoms. In certain instances, the thickening of liquids may be requisite to prevent aspiration16.
Restricting alcohol and caffeine intake can help mitigate symptoms, as these substances may irritate the esophagus. Implementing hydration strategies, such as the utilization of thickened beverages, is crucial for ensuring safe fluid intake while managing dysphagia16.
Speech and language therapy provides invaluable techniques and exercises aimed at enhancing muscle coordination necessary for swallowing. These therapeutic interventions are instrumental in the comprehensive management of swallowing disorders16.
Through the implementation of these lifestyle modifications and management strategies, individuals with esophageal dysphagia can substantially enhance their quality of life and diminish the risk of associated complications16.
Dietary Adjustments and Nutrition
Dietary adjustments are paramount in managing esophageal dysphagia. Patients frequently necessitate specialized dysphagia diets to guarantee safe swallowing and adequate nutrition. These diets concentrate on food consistency and texture modifications to avert complications and enhance quality of life.
Food Texture Modifications
Modifying food textures is a pivotal strategy in dysphagia management. Soft, pureed, or minced foods are commonly advised to facilitate swallowing. Over half of dysphagia patients require significantly modified food textures to fulfill their dietary needs17. The International Dysphagia Diet Standardisation Initiative (IDDSI) offers guidelines for food textures appropriate for various dysphagia levels.
Thickening Liquids
Thickening liquids is another critical aspect of dysphagia diet management. This practice aids in preventing aspiration by slowing the flow of liquids during swallowing. Thickeners can be added to diverse beverages to attain the correct consistency for safe consumption.

Nutritional Considerations
Nutritional support is essential for dysphagia patients, as the condition can lead to malnutrition. A study revealed that 39.8% of children with swallowing disorders did not meet their total energy expenditure, indicating a high risk of malnutrition17. In elderly populations, malnutrition affects 17-20% of those living alone with dysphagia, increasing to 37-67% among hospitalized seniors18.
Dietitians often recommend nutrient-dense foods and supplements to ensure adequate nutrition. For some patients, alternative feeding methods like nasogastric tubes or gastrostomy may be necessary. After individualized speech therapy and nutritional rehabilitation, patients can experience significant improvements in their energy coverage17.
| Age Group | Dysphagia Prevalence |
|---|---|
| 65-70 years | 13% |
| 70-79 years | 16% |
| 80+ years | 33% |
Dysphagia significantly affects a substantial portion of the elderly population, with prevalence increasing with age18. This highlights the necessity of tailored nutritional strategies for different age groups.
Complications and Prevention Strategies
Untreated esophageal dysphagia can precipitate severe complications. Aspiration pneumonia, malnutrition, and dehydration are among the gravest dysphagia complications. The risk of these issues escalates with the severity of swallowing difficulties19.
Prevention strategies pivot on the proper management of underlying conditions and strict adherence to treatment plans. Regular consultations with healthcare providers are imperative for monitoring progress and adjusting interventions as necessary. Safe swallowing techniques are paramount in preventing aspiration.
Dietary modifications are crucial in managing dysphagia and mitigating malnutrition risks. Patients may benefit from consuming food slowly, chewing thoroughly, and selecting soft foods. Additionally, sitting upright while eating and refraining from talking during swallowing can prevent complications20.
Cancer treatments, such as radiation therapy or surgery to the mouth, jaw, throat, or esophagus, significantly contribute to swallowing problems in a substantial percentage of patients. The prevalence of patient-reported dysphagia in cancer patients is estimated between 1141 and 1150 cases per 100,000 individuals21.
| Complication | Prevention Strategy |
|---|---|
| Aspiration Pneumonia | Proper positioning during meals, thickened liquids |
| Malnutrition | Nutrient-dense foods, small frequent meals |
| Dehydration | Modified fluid intake, ice chips |
Education on proper food preparation and eating habits is critical for both patients and caregivers. In some instances, preventive measures may involve avoiding certain medications known to affect swallowing or exacerbate reflux. Regular dental check-ups are also vital in preventing oral health issues that may exacerbate dysphagia symptoms.
Living with Esophageal Dysphagia
Esophageal dysphagia profoundly influences an individual’s quality of life, manifesting across all age spectrums but predominantly affecting the elderly and those afflicted with specific neurological conditions22. In the United States, a staggering 15-22% of individuals over 50 residing in the community suffer from dysphagia, with prevalence escalating to 40-60% within nursing home settings23.
Daily Management Tips
Effective management of esophageal dysphagia necessitates the adoption of robust coping strategies. These include:
- Maintaining proper posture during meals
- Utilizing adaptive utensils when necessary
- Ensuring hydration to prevent complications
- Modifying food textures for enhanced swallowability
It is imperative to recognize symptoms such as coughing or gagging during swallowing, feeling food lodged in the throat, or experiencing pain during the act of swallowing22. Failure to address dysphagia can precipitate severe complications, including choking, dehydration, malnutrition, and aspiration pneumonia22.
Support Resources
Support for individuals grappling with swallowing disorders is accessible through diverse channels:
- Support groups
- Online forums
- Organizations such as the National Foundation of Swallowing Disorders
Healthcare professionals may direct individuals with dysphagia to specialists including speech and language pathologists, otolaryngologists, gastroenterologists, or neurologists for comprehensive evaluation and treatment22.
Long-term Outlook
The prognosis for esophageal dysphagia varies based on the underlying cause and the efficacy of treatment. Regular consultations with healthcare providers are critical for monitoring progress and tailoring treatment plans. With diligent management, many patients can experience significant enhancements in their quality of life.
| Aspect | Impact on Quality of Life | Management Strategy |
|---|---|---|
| Physical Challenges | Difficulty swallowing, altered dietary habits | Food texture modifications, adaptive utensils |
| Psychosocial Strain | Emotional distress, social isolation | Support groups, counseling |
| Financial Burden | Increased healthcare costs, potential loss of work | Financial counseling, insurance navigation |
By addressing these aspects comprehensively, individuals with esophageal dysphagia can better manage their condition and enhance their overall quality of life.
Conclusion
Esophageal dysphagia embodies a formidable challenge within the realm of swallowing disorder management. The imperative for early detection and intervention cannot be overstated, as it serves as a bulwark against malnutrition, weight loss, and aspiration pneumonia24. Immediate medical intervention can profoundly elevate the quality of life for those grappling with this affliction.
Diagnostic modalities such as endoscopy, barium swallow studies, and esophageal manometry are indispensable in uncovering the root causes of dysphagia25. These methodologies empower healthcare professionals to devise personalized treatment strategies, thereby optimizing esophageal health outcomes. The spectrum of treatment modalities spans from pharmacological interventions for acid reflux to surgical interventions for esophageal anomalies, with the deployment of feeding tubes reserved for the most severe cases24.
The imperative for heightened swallowing disorder awareness cannot be overstated, as it underpins early diagnosis. Patients must remain vigilant to symptoms such as coughing during meals, throat clearing, or a sensation of obstruction during swallowing26. Adherence to safe swallowing practices, including the adoption of proper posture and modifications in food texture, can significantly mitigate symptoms. As research continues to evolve and treatment modalities advance, many individuals with esophageal dysphagia can sustain good nutrition and lead enriched lives.
FAQ
What is esophageal dysphagia?
What are the common causes of esophageal dysphagia?
What are the primary symptoms of esophageal dysphagia?
How is esophageal dysphagia diagnosed?
What treatment options are available for esophageal dysphagia?
Are there lifestyle modifications that can help manage esophageal dysphagia?
What dietary adjustments are recommended for patients with esophageal dysphagia?
What are the potential complications of untreated esophageal dysphagia?
What is the long-term outlook for patients with esophageal dysphagia?
Source Links
- Dysphagia – Symptoms and causes – https://www.mayoclinic.org/diseases-conditions/dysphagia/symptoms-causes/syc-20372028
- Dysphagia Causes, Symptoms, and Treatment Options – https://www.tgh.org/institutes-and-services/conditions/dysphagia
- Oropharyngeal dysphagia: Etiology and pathogenesis – https://www.uptodate.com/contents/oropharyngeal-dysphagia-etiology-and-pathogenesis/print
- Dysphagia – https://www.beaconhealthsystem.org/library/diseases-and-conditions/dysphagia/
- Difficulty Swallowing (Dysphagia): Types, Causes & Treatment – https://www.hoag.org/specialties-services/digestive-health/diseases-conditions/dysphagia/
- Swallowing difficulty – UF Health – https://ufhealth.org/conditions-and-treatments/swallowing-difficulty
- What Is an Esophageal Stricture? – https://my.clevelandclinic.org/health/diseases/21456-esophageal-strictures
- Esophagitis – Symptoms and causes – https://www.mayoclinic.org/diseases-conditions/esophagitis/symptoms-causes/syc-20361224
- Dysphagia – https://www.sgihealth.com/patients/digestive-health-library/dysphagia/
- Dysphagia and GERD: Easing Your Difficulty in Swallowing – https://www.healthline.com/health/gerd/dysphagia
- Approach Considerations, Imaging Studies, Endoscopy – https://emedicine.medscape.com/article/2212409-workup
- Swallowing Evaluations | doctorlansford.com – https://www.doctorlansford.com/diagnostics-swallow-evaluations
- Diagnostic Approach to Dysphagia — NP Reasoning – https://www.npreasoning.com/diagnostic-imaging/diagnostic-approach-to-dysphagia
- Dysphagia and Deglutition Clinic – https://www.hopkinsmedicine.org/otolaryngology/specialty-areas/swallowing-center/dysphagia-and-deglutition-clinic
- Dysphagia – Care at Mayo Clinic – https://www.mayoclinic.org/diseases-conditions/dysphagia/care-at-mayo-clinic/mac-20372039
- Effective Clinical Strategies for Managing Swallowing Disorders – https://www.beckerentandallergy.com/blog/strategies-for-swallowing-disorders
- Nutritional Issues in Children with Dysphagia – https://pmc.ncbi.nlm.nih.gov/articles/PMC11174107/
- Food Processing and Nutrition Strategies for Improving the Health of Elderly People with Dysphagia: A Review of Recent Developments – https://pmc.ncbi.nlm.nih.gov/articles/PMC10814519/
- 10 Essential Strategies for Managing Dysphagia – Medbridge Blog – https://www.medbridge.com/blog/2024/08/10-essential-strategies-for-managing-dysphagia/
- Dysphagia and Mental Illness: Causes and Symptoms – https://www.verywellhealth.com/esophageal-dysphagia-5097624
- Swallowing Problems | Managing Cancer-related Side Effects – https://www.cancer.org/cancer/managing-cancer/side-effects/eating-problems/swallowing-problems.html
- Dysphagia Tests: MedlinePlus Medical Test – https://medlineplus.gov/lab-tests/dysphagia-tests/
- Hypocalcemia as an Independent Cause of Esophageal Dysphagia: A Case Report – https://pmc.ncbi.nlm.nih.gov/articles/PMC11524542/
- Understanding Dysphagia: Causes, Symptoms, Diagnosis, and Treatment In Thanc Hospital-Chennai – https://thanchospital.com/understanding-dysphagia-thanc-chennai/
- Swallowing Problems (Dysphagia) Causes, Symptoms, Treatment – https://www.medicinenet.com/swallowing/article.htm
- Trouble Swallowing After Stroke (Dysphagia) – https://www.stroke.org/en/about-stroke/effects-of-stroke/physical-effects/dysphagia