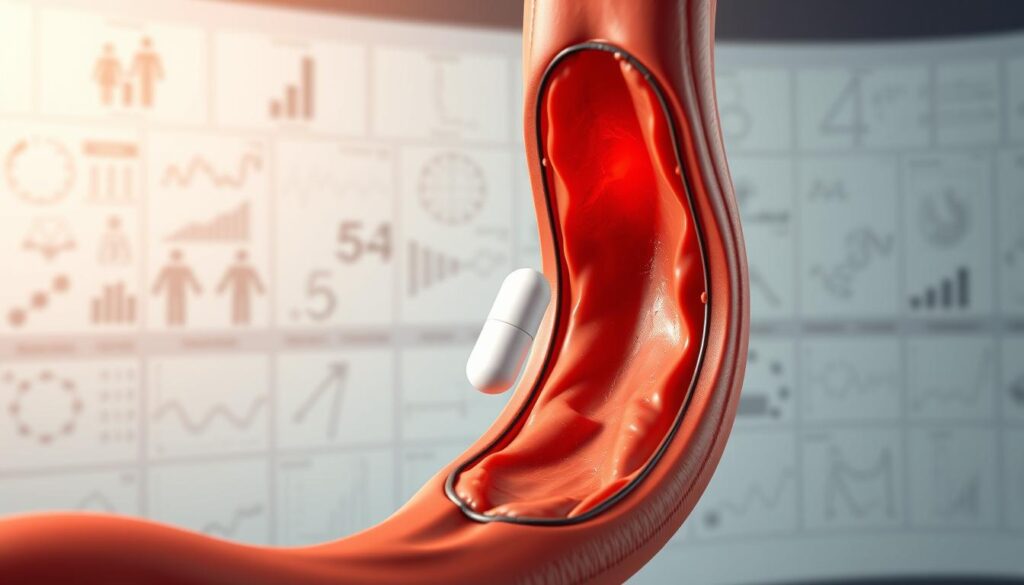
The advent of vonoprazan, a potassium-competitive acid blocker (P-CAB), heralds a paradigm shift in the treatment of erosive esophagitis (EE). This innovation challenges the supremacy of proton pump inhibitors (PPIs), such as lansoprazole, in the management of gastroesophageal reflux disease (GERD)1.
A landmark trial, PHALCON-EE, involved 1,020 participants to evaluate the efficacy of vonoprazan against lansoprazole. The results indicated that vonoprazan achieved noninferiority endpoints for healing by week 8, surpassing lansoprazole’s efficacy1.
Notably, vonoprazan demonstrated superior efficacy at week 2 in patients with severe EE (LA Grade C/D lesions). This breakthrough suggests a new frontier in treating cases where traditional PPIs often fail1.
The FDA’s approval of vonoprazan for EE treatment in November 2023 signifies a significant milestone. It marks the first approval of a P-CAB for this indication in the United States. This approval heralds a new era for patients who have not responded to conventional PPI therapy1.
Key Takeaways
- Vonoprazan is a new P-CAB drug approved for EE treatment
- It shows noninferiority to lansoprazole in overall EE healing
- Vonoprazan is superior in treating severe EE cases
- FDA approval in 2023 marks a shift in EE treatment options
- P-CABs may offer benefits for PPI-resistant cases
Understanding Erosive Esophagitis (EE) and Its Impact
Erosive esophagitis (EE) represents a severe manifestation of gastroesophageal reflux disease (GERD), characterized by inflammation and erosive alterations in the esophageal mucosa. This condition pervades millions globally, with a global age-standardized prevalence of 8,818.9 per 100,000 population2.
What is Erosive Esophagitis
EE arises from the recurrent reflux of stomach acid into the esophagus, inducing damage to its protective lining. This acid reflux precipitates esophageal inflammation, potentially culminating in the formation of ulcers or erosions. In Western nations, EE constitutes approximately 30% of GERD cases2.
Prevalence and Risk Factors
The prevalence of GERD exhibits variability across the globe, with the United States reporting a rate of 12,608.2 per 100,000 population in 20172. Obesity, smoking, specific medications, and hiatal hernia are identified risk factors for EE. Age also plays a role, with patients’ mean ages ranging from 51 to 58 years in recent studies3.
Clinical Manifestations and Symptoms
Symptoms of EE often mirror those of GERD, encompassing heartburn, regurgitation, and difficulty swallowing. The severity of EE is graded using the Los Angeles (LA) system, with approximately 80% of cases categorized as milder LA grade A/B3. If left untreated, EE can escalate to complications such as strictures or Barrett’s esophagus, affecting 6% to 8% of GERD patients in Western countries2.
Comprehending the impact of EE is imperative for effective management. Recent studies comparing treatment options have included 2,554 patients across four randomized controlled trials, underscoring the condition’s significance in clinical research3.
Current Treatment Landscape for Erosive Esophagitis
Proton pump inhibitors (PPIs) are the foundational treatment for erosive esophagitis (EE). Medications such as lansoprazole are widely used due to their efficacy in acid suppression1. They have shown remarkable success in treating milder forms of EE, including Los Angeles grades A and B1.
Despite their effectiveness, PPIs face challenges in treating severe EE cases. Healing rates for Los Angeles Grade C/D lesions lag behind those of milder forms1. This gap in efficacy has spurred research into alternative treatments, leading to the development of potassium-competitive acid blockers (P-CABs) like vonoprazan.
The PHALCON-EE trial, involving 1,020 participants, compared vonoprazan to lansoprazole in EE treatment. Vonoprazan demonstrated noninferiority in overall healing and superiority in treating severe cases1. These findings suggest a shift in the treatment paradigm, potentially favoring vonoprazan for difficult-to-treat EE cases.
| Treatment | Overall Healing (8 weeks) | LA Grade C/D Healing (2 weeks) | Maintenance (24 weeks) |
|---|---|---|---|
| Vonoprazan | Noninferior | Superior | Superior (LA Grade C/D) |
| Lansoprazole | Standard | Standard | Standard |
While PPIs remain the first-line treatment, emerging data on P-CABs like vonoprazan are reshaping the EE management landscape. The FDA’s approval of vonoprazan in November 2023 marks a significant milestone, providing a new option for patients with persistent symptoms or severe disease1. Cost considerations and long-term safety data will play critical roles in determining the widespread adoption of these newer agents in clinical practice1.
Vonoprazan vs Lansoprazole for Erosive Esophagitis
The advent of novel pharmacotherapies has revolutionized the treatment of erosive esophagitis. This discourse juxtaposes vonoprazan, a potassium-competitive acid blocker (P-CAB), against lansoprazole, a proton pump inhibitor (PPI), in their methodologies for addressing this affliction.
Mechanism of Action Differences
Vonoprazan and lansoprazole diverge in their acid suppression mechanisms. Vonoprazan, a P-CAB, reversibly inhibits the H+,K+-ATPase enzyme, irrespective of pH levels. In contrast, lansoprazole, a PPI, irreversibly blocks this enzyme, necessitating acid activation for efficacy.
Dosing Requirements and Flexibility
The PHALCON-EE trial elucidated the efficacy of 20 mg of vonoprazan versus 30 mg of lansoprazole for healing, and 10 mg or 20 mg of vonoprazan versus 15 mg of lansoprazole for maintenance1. Vonoprazan’s pH-independent action facilitates more adaptable dosing regimens, potentially augmenting patient compliance.
Speed of Onset and Duration
Vonoprazan exhibited expedited symptom alleviation, with enhanced heartburn resolution on day 1 and statistically significant improvement by day 7, surpassing most PPIs1. The PHALCON-EE trial demonstrated vonoprazan’s superiority in healing severe erosive esophagitis (LA Grade C/D) by week 21.
| Aspect | Vonoprazan (P-CAB) | Lansoprazole (PPI) |
|---|---|---|
| Mechanism | Reversible, pH-independent | Irreversible, acid-activated |
| Onset of Action | Faster (Day 1-7) | Slower |
| Efficacy in Severe EE | Superior by Week 2 | Less effective early on |
Despite vonoprazan’s promising efficacy, its elevated cost compared to PPIs may deter its adoption as a primary treatment1. The VISION trial’s long-term safety data revealed no novel concerns after 3 years, albeit with increased gastric cellular hyperplasia with vonoprazan administration1.
Clinical Efficacy in EE Healing
Erosive esophagitis (EE) impacts approximately 10% of the Asian populace, manifesting as mucosal disruptions within the esophagus4. The efficacy of treatment varies, with a 10-15% failure rate in achieving healing within an 8-week timeframe using proton pump inhibitors (PPIs)4.
Short-term Healing Rates
Vonoprazan exhibits superior short-term healing efficacy compared to lansoprazole, predominantly in severe EE cases. In LA grade C/D EE, vonoprazan’s risk ratio is 2.72 (95% CI, 1.10-6.73) over lansoprazole5. This highlights vonoprazan’s enhanced EE healing rates in complex scenarios.
Long-term Maintenance Therapy
Maintenance therapy is imperative due to EE recurrence rates reaching up to 90% upon PPI discontinuation4. A 24-week study revealed vonoprazan’s superiority over lansoprazole in preventing EE recurrence. The recurrence rates were 13.3% for vonoprazan 10 mg, 12.3% for vonoprazan 20 mg, and 25.5% for lansoprazole4.
| Medication | EE Recurrence Rate |
|---|---|
| Vonoprazan 10 mg | 13.3% |
| Vonoprazan 20 mg | 12.3% |
| Lansoprazole | 25.5% |
Effectiveness in Severe Cases (LA Grade C/D)
Vonoprazan stands out in treating severe erosive esophagitis. Pooled analyses indicate a risk ratio of 2.97 compared to lansoprazole and 3.51 versus omeprazole for LA grade C/D EE5. This emphasizes vonoprazan’s effectiveness in severe EE cases, providing hope for patients with challenging conditions.
Overall, vonoprazan showcases superior clinical efficacy in EE healing, with notable advantages in severe cases and long-term maintenance therapy. Its performance exceeds that of traditional PPIs, positioning it as a promising treatment option for EE45.
Safety Profiles and Considerations
Vonoprazan and lansoprazole exhibit comparable safety profiles in the treatment of erosive esophagitis. Clinical studies indicate that vonoprazan offers enhanced acid inhibition compared to traditional proton pump inhibitors such as lansoprazole6. This increased potency enables effective management of acid-related disorders, including erosive esophagitis6.
Regarding adverse events, vonoprazan treatment reported a 33.3% rate of treatment-emergent adverse events (AEs), marginally higher than the 26.4% observed with PPIs7. Gastrointestinal discomfort was noted in less than 5% of patients using vonoprazan, with a 2% incidence of serious adverse events6.
Long-term safety considerations for both medications include the risks associated with prolonged acid suppression. Vonoprazan maintains an intragastric pH level.
Regarding drug interactions, vonoprazan’s efficacy persists across diverse populations, including those with different CYP2C19 genotypes, a factor affecting traditional PPI efficacy6. This suggests potentially fewer drug interactions compared to lansoprazole.
| Parameter | Vonoprazan | Lansoprazole |
|---|---|---|
| Treatment-emergent AEs | 33.3% | 26.4% |
| Intragastric pH | ~16 hours | ~8 hours |
| Gastrointestinal discomfort | Not specified | |
| Serious adverse events | 2% | Not specified |
Cost-Effectiveness and Accessibility
The economic implications of treating erosive esophagitis with vonoprazan versus lansoprazole are of utmost importance for both patients and healthcare providers. This section delves into the financial aspects, insurance coverage, and market availability of these treatments.
Insurance Coverage
Insurance coverage for vonoprazan and lansoprazole exhibits variability. Lansoprazole, a well-established proton pump inhibitor, is frequently covered by most insurance plans. In contrast, vonoprazan, a newer medication, may face limited coverage. Patients must verify their insurance coverage with their providers to understand their options.
Treatment Costs Comparison
The cost disparity between vonoprazan and lansoprazole is substantial. PPIs such as lansoprazole, due to their long-standing market presence and availability of generic versions, are generally more affordable. On the other hand, vonoprazan, a newer drug, commands a higher price. The annual economic burden of gastroesophageal reflux disease (GERD) in the United States is estimated at $40 billion, underscoring the necessity for cost-effective treatments8.
Market Availability
Lansoprazole is widely accessible as both prescription and over-the-counter medication across many countries. In contrast, vonoprazan’s market access is more restricted, being a relatively recent entrant. Availability varies by region, with some countries approving its use while others are in the evaluation phase.
Despite the higher drug costs, vonoprazan may offer a more cost-effective solution in the long term. Its superior efficacy in treating severe cases of erosive esophagitis could potentially reduce the need for prolonged treatment or additional interventions, offsetting the initial higher cost. Yet, more detailed cost-effectiveness studies are imperative to fully grasp its economic impact on healthcare systems and patients.
Special Patient Populations and Considerations
The treatment of erosive esophagitis necessitates a refined strategy, given the heterogeneity of patient demographics. The interplay between ethnic variations and genetic predispositions significantly impacts therapeutic efficacy, underscoring the imperative for a personalized approach to medicine.
Asian Population Response
Research indicates that Asian patients exhibit distinct responses to treatments for erosive esophagitis. A comparative analysis revealed that vonoprazan and lansoprazole demonstrated comparable efficacy in this demographic, with healing rates of 92.4% and 91.3% respectively2. This minimal disparity suggests that genetic determinants may influence drug efficacy within this population.
CYP2C19 Polymorphism Impact
The CYP2C19 enzyme is instrumental in drug metabolism, with over 80% of lansoprazole metabolism attributed to it9. Genetic polymorphisms in CYP2C19, prevalent in Asian populations, can expedite PPI metabolism, potentially diminishing treatment efficacy.
Vonoprazan, on the other hand, is not predominantly metabolized by CYP2C19. This characteristic may confer an advantage in patients with rapid PPI metabolism, underscoring the significance of personalized medicine in erosive esophagitis treatment.
These insights underscore the necessity for healthcare providers to consider ethnic variations and genetic factors when selecting between vonoprazan and lansoprazole. By customizing treatments to individual patient characteristics, we can enhance outcomes and elevate patient satisfaction in the management of erosive esophagitis.
Treatment Duration and Monitoring
The management of erosive esophagitis necessitates a meticulous approach to treatment duration and patient surveillance. The standard initial treatment duration for GERD employing PPIs is typically 4-8 weeks10. A comparative study between tegoprazan and lansoprazole revealed remarkable healing rates at 4 weeks, with tegoprazan achieving 95.2% efficacy, surpassing lansoprazole’s 86.2%10.
Preventing relapse through long-term acid suppression is critical. Vonoprazan-based regimens have demonstrated superior efficacy across various gastrointestinal disorders. In the context of erosive esophagitis, vonoprazan exhibits healing rates ranging from 92.3% to 99.0%, marginally outperforming lansoprazole’s 93.2% to 95.5% efficacy7.
Follow-up care is indispensable for evaluating treatment efficacy and making necessary adjustments. Regular endoscopic assessments are vital for monitoring healing and identifying any complications. Patients undergoing long-term acid suppression must be closely monitored for side effects and nutritional deficiencies.
| Medication | Initial Treatment Duration | Healing Rate at 4 Weeks | Maintenance Therapy Efficacy |
|---|---|---|---|
| Vonoprazan | 4-8 weeks | 95.2% (as tegoprazan) | 92.3% – 99.0% |
| Lansoprazole | 4-8 weeks | 86.2% | 93.2% – 95.5% |
Vonoprazan’s potent acid inhibition, estimated to be 350 times stronger than traditional PPIs, suggests its utility in intensive acid suppression scenarios7. Yet, clinicians must weigh the slightly higher rate of treatment-emergent adverse events with vonoprazan (33.3%) against PPIs (26.4%) when designing long-term therapy plans7.
Emerging Research and Future Directions
The domain of erosive esophagitis treatment is witnessing exponential growth, with a concentration on pioneering drug development and prospective treatments. Vonoprazan, a potent acid suppressant, stands at the vanguard of these advancements.
Ongoing Clinical Trials
Recent investigations have unveiled encouraging outcomes for vonoprazan in the treatment of erosive esophagitis. A randomized trial, encompassing 60 participants, revealed substantial symptom amelioration with both 10 mg and 20 mg doses of vonoprazan11. The Global Overall Symptoms Scale (GOSS) scores exhibited a significant decline over an 8-week period, underscoring the efficacy of symptom relief11.
Vonoprazan’s efficacy transcends mere symptom alleviation. In the realm of first-line Helicobacter pylori eradication, vonoprazan-based regimens achieve eradication rates ranging from 89.0% to 97.4%, outperforming traditional proton pump inhibitor (PPI) regimens7. For erosive esophagitis, vonoprazan exhibits healing rates of 92.3% to 99.0%, on par with lansoprazole’s 93.2% to 95.5%7.
New Development Areas
Researchers are delving into vonoprazan’s applicability in diverse gastrointestinal afflictions. Its efficacy in healing post-endoscopic submucosal dissection ulcers (94.9%) surpasses that of PPIs (78%)7. Vonoprazan’s rapid onset and prolonged duration of action, with a median time to maximum concentration of 1-2 hours and an elimination half-life of up to nine hours, position it as a formidable candidate for future therapeutic applications7.
As drug development continues, vigilance regarding safety is imperative. The incidence of treatment-emergent adverse events for vonoprazan (33.3%) marginally exceeds that of PPIs (26.4%), necessitating continuous surveillance7. Future clinical trials may investigate optimal dosing regimens and long-term safety profiles to further delineate vonoprazan’s role in the management of erosive esophagitis.
Making the Treatment Choice
The process of treatment decision-making for erosive esophagitis necessitates a meticulous evaluation of multiple variables. Healthcare professionals must meticulously assess the advantages and disadvantages of various pharmacotherapies to ensure patient-centered care. Recent investigations have illuminated the superiority of newer agents, such as vonoprazan, over traditional treatments like lansoprazole.
First-line Treatment Considerations
In the selection of initial therapy for erosive esophagitis, clinicians must consider the severity of the disease, patient-specific characteristics, and treatment objectives. Clinical guidelines frequently advocate for proton pump inhibitors (PPIs) as the first line of treatment. The FDA’s approval of vonoprazan has introduced a novel alternative, demonstrating enhanced healing efficacy of 81% compared to 63% for lansoprazole over an 8-week treatment duration12.
Choosing Vonoprazan Over Lansoprazole
Vonoprazan may be the preferred choice for severe erosive esophagitis (LA Grade C/D) or for patients with a history of PPI failure. Its efficacy in symptom reduction is reported at 85%, surpassing lansoprazole’s 70% efficacy12. A recent evaluation employing the EVIDEM framework, which encompasses 13 criteria, revealed a value contribution of 0.59 for vonoprazan, underscoring its benefits in specific clinical contexts13.
Patient-centered care mandates a collaborative approach, considering factors such as cost, convenience, and individual preferences. A holistic strategy, integrating both clinical guidelines and patient-specific considerations, is essential for achieving optimal outcomes in the management of erosive esophagitis.
Conclusion
The comparative analysis between vonoprazan and lansoprazole in the treatment of erosive esophagitis (EE) uncovers profound implications for clinical practice. Vonoprazan exhibits superior efficacy, predominantly in severe EE cases. A study involving 703 patients revealed that vonoprazan 20 mg exhibited lower EE recurrence rates (12.3%) compared to lansoprazole (25.5%) over a 24-week period4. This enhanced efficacy was corroborated in a pooled analysis, where vonoprazan surpassed lansoprazole with a risk ratio of 2.97 for initial efficacy and 8.39 for maintenance efficacy5.
Patient outcomes with vonoprazan showed marked improvement, most prominently in maintenance therapy. At 12 weeks, vonoprazan 20 mg demonstrated a lower EE recurrence rate (10.0%) compared to lansoprazole (35.0%)4. The surface under the cumulative probability ranking (SUCRA) for initial and maintenance efficacy ranked vonoprazan highest at 0.89 and 0.87 respectively, indicating its suitability as a first-line treatment for EE5.
The safety profiles of vonoprazan and lansoprazole were found to be comparable. Treatment-emergent adverse events occurred at similar rates: 69.0% for vonoprazan 20 mg and 65.3% for lansoprazole4. No significant differences in risk for short-term or long-term adverse events were identified among 5026 patients analyzed5. These results suggest that vonoprazan could serve as a safe and effective alternative to lansoprazole, with particular benefits for patients with severe EE or those resistant to proton pump inhibitors.
FAQ
What is erosive esophagitis (EE) and how does it differ from GERD?
How do vonoprazan and lansoprazole differ in their mechanisms of action?
Are there differences in efficacy between vonoprazan and lansoprazole for treating severe EE (LA Grade C/D)?
How do the safety profiles of vonoprazan and lansoprazole compare?
Are there differences in cost and accessibility between vonoprazan and lansoprazole?
How does the response to vonoprazan and lansoprazole differ in Asian populations?
What is the recommended duration of treatment for EE with vonoprazan or lansoprazole?
Are there ongoing clinical trials comparing vonoprazan to other treatments for EE?
When should a clinician consider prescribing vonoprazan over lansoprazole for EE?
Can vonoprazan and lansoprazole be used interchangeably for EE treatment?
Source Links
- Will Vonoprazan Be the New First-Line Erosive Esophagitis Treatment? – https://www.gastroenterologyadvisor.com/features/erosive-esophagitis-treatment-vonoprazan-vs-ppis-first-line-therapy/
- Treating Erosive Esophagitis With Potassium-Competitive Acid Blockade – https://www.gastroenterologyadvisor.com/cch/erosive-esophagitis-gerd-potassium-competitive-acid-blockade-vonoprazan-lansoprazole/
- A systematic review with meta‐analysis: Efficacy and safety of potassium‐competitive acid blocker compared with proton pump inhibitor in the maintenance of healed erosive esophagitis – https://pmc.ncbi.nlm.nih.gov/articles/PMC10958938/
- Vonoprazan 10 mg or 20 mg vs. lansoprazole 15 mg as maintenance therapy in Asian patients with healed erosive esophagitis: A randomized controlled trial – https://pmc.ncbi.nlm.nih.gov/articles/PMC11046018/
- Healing Grade C/D Esophagitis Best Achieved With Vonoprazan vs PPIs – https://www.gastroenterologyadvisor.com/news/healing-grade-cd-esophagitis-best-achieved-with-vonoprazan-vs-ppis/
- Potassium-competitive Acid Blockers: Current Clinical Use and Future Developments – Current Gastroenterology Reports – https://link.springer.com/article/10.1007/s11894-024-00939-3
- A Comprehensive Review on the Efficacy and Safety of Vonoprazan in the Management of Gastric Acid-Related Diseases – https://pmc.ncbi.nlm.nih.gov/articles/PMC11330167/
- Economic evaluation of proton pump inhibitors in patients with gastro-oesophageal reflux disease: a systematic review – https://pmc.ncbi.nlm.nih.gov/articles/PMC11664378/
- Clinical Implications of Proton Pump Inhibitors and Vonoprazan Micro/Nano Drug Delivery Systems for Gastric Acid-Related Disorders and Imaging – https://www.ntno.org/v08p0535.htm
- Comparison of Tegoprazan and Lansoprazole in Patients With Erosive Esophagitis up to 4 Weeks: A Multi‐Center, Randomized, Double‐Blind, Active‐Comparator Phase 4 Trial – https://pmc.ncbi.nlm.nih.gov/articles/PMC11650551/
- Efficacy of Vonoprazan 10 mg and 20 mg for Patients With Proton Pump Inhibitor‐Refractory Functional Dyspepsia: A Double‐Blinded, Randomized Study – https://pmc.ncbi.nlm.nih.gov/articles/PMC11659636/
- Approach Considerations, Reflux Esophagitis, Infectious Esophagitis – https://emedicine.medscape.com/article/174223-treatment
- Evaluating vonoprazan and tegoprazan for gastroesophageal reflux disease treatment in Chinese Healthcare: an EVIDEM framework analysis – BMC Gastroenterology – https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-024-03297-6