Gastrointestinal bleeding remains a critical concern in medical practice, requiring precise interventions to ensure patient safety. One of the most effective tools for managing this condition is the use of mechanical hemostasis devices. These small, clip-like instruments play a vital role in controlling bleeding during diagnostic and therapeutic procedures.
First introduced in 1975, these devices have evolved significantly, offering improved precision and reliability. Modern variants include through-the-scope (TTS) and over-the-scope (OTSC) systems, designed for different clinical scenarios. Their application spans esophageal, gastric, duodenal, and colonic interventions, reducing the need for invasive surgeries.
By minimizing surgical risks and improving recovery times, these tools have become indispensable in gastroenterology. Their clinical significance lies in their ability to address both acute and delayed bleeding episodes effectively.
Key Takeaways
- Mechanical hemostasis devices are essential for managing gastrointestinal bleeding.
- Modern variants include TTS and OTSC systems for different medical needs.
- These tools reduce the necessity for invasive surgical procedures.
- They are widely used in esophageal, gastric, duodenal, and colonic treatments.
- Patient outcomes improve significantly with their application.
Introduction to Hemoclips in Endoscopy
The evolution of mechanical hemostasis tools has transformed treatment approaches for digestive tract bleeding. These devices, designed to clamp bleeding vessels, offer a minimally invasive alternative to surgery. Their precision reduces tissue damage and accelerates recovery.
Defining Mechanical Clipping Systems
Mechanical hemostasis devices are small, clip-like instruments deployed during endoscopic procedures. They compress blood vessels to stop bleeding without thermal or chemical intervention. Modern variants include through-the-scope (TTS) and over-the-scope (OTSC) systems, each suited for specific clinical scenarios.
Historical Milestones
Developed in 1975, the first clipping device addressed acute gastrointestinal bleeding management. Key advancements followed:
- 1993: Commercial TTS systems enabled widespread clinical use.
- 2007: OTSC devices improved outcomes for refractory bleeding and perforations.
- Recent Innovations: Multi-fire devices and repositionable clips expanded applications.
Today, these tools are used preventively, such as post-polypectomy, showcasing their versatility in treatment gastrointestinal bleeding.
How Hemoclips Endoscopy Works
Modern endoscopic tools offer precise control over bleeding vessels through advanced clipping mechanisms. These devices compress tissue to occlude blood flow, enabling rapid hemostasis without thermal or chemical agents.
Mechanism of Action
Clipping systems mechanically seal vessels by applying direct pressure. The compression triggers natural clotting, reducing rebleeding risks. This method is particularly effective for upper gastrointestinal lesions with active hemorrhage.
Types of Clips: Through-the-Scope vs. Over-the-Scope
Through-the-Scope (TTS): Fits standard endoscopes (8–16mm working length). Ideal for accessible lesions due to 225–250cm insertion range.
Over-the-Scope Clips (OTSC): Feature an 11mm nitinol ring for 360° compression. Success rates reach 85% for refractory bleeding and 66% for anastomotic leaks.
- OTSC Advantages: Hexagonal design ensures secure closure of fibrotic ulcers or perforations >2cm.
- Deployment Note: Requires scope removal/reinsertion, unlike TTS systems.
Clinical Applications of Hemoclips
Clinical outcomes improve when the right technique matches the bleeding source. Mechanical clipping systems are tailored to address specific vascular lesions across the gastrointestinal tract. Their versatility makes them indispensable in both emergency and elective settings.
Bleeding Peptic Ulcers
For ulcers with visible vessels, clips achieve hemostasis in 90% of cases. They compress the bleeding point directly, minimizing tissue damage. Studies show lower rebleeding rates compared to thermal methods.
Mallory-Weiss Syndrome
These mucosal tears often respond to clipping when located near the gastroesophageal junction. The device seals the laceration, reducing transfusion needs. Success rates exceed 85% in acute episodes.
Dieulafoy’s Lesion
This rare but severe condition involves aberrant submucosal arteries. Clips provide precise vessel occlusion, with efficacy rates of 87–94%. They outperform epinephrine injections in preventing recurrent bleeding.
Colonic Diverticular Bleeding
For colonic diverticular bleeding, clip placement targets the base of the diverticulum. It localizes the vessel and serves as an anatomical marker for angiography if needed. Technical challenges include identifying bleeding stigmata in the right colon.
“Clipping reduces 1-year rebleeding rates to 13.6%, though endoscopic band ligation remains superior at 6.8% for select cases.”
| Intervention | Acute Hemostasis Rate | 1-Year Rebleeding |
|---|---|---|
| Mechanical Clipping | 87–100% | 13.6% |
| Band Ligation | 92–98% | 6.8% |
Left-sided lesions are more accessible, while right-colon bleeding demands advanced endoscopic skills. Clips offer a balance of speed and precision in these scenarios.
Techniques for Endoscopic Hemoclip Placement
Precision in mechanical clipping requires mastering specific deployment techniques to ensure optimal outcomes. Proper placement minimizes rebleeding risks and adapts to anatomical challenges, such as fibrotic tissue or awkward angles.
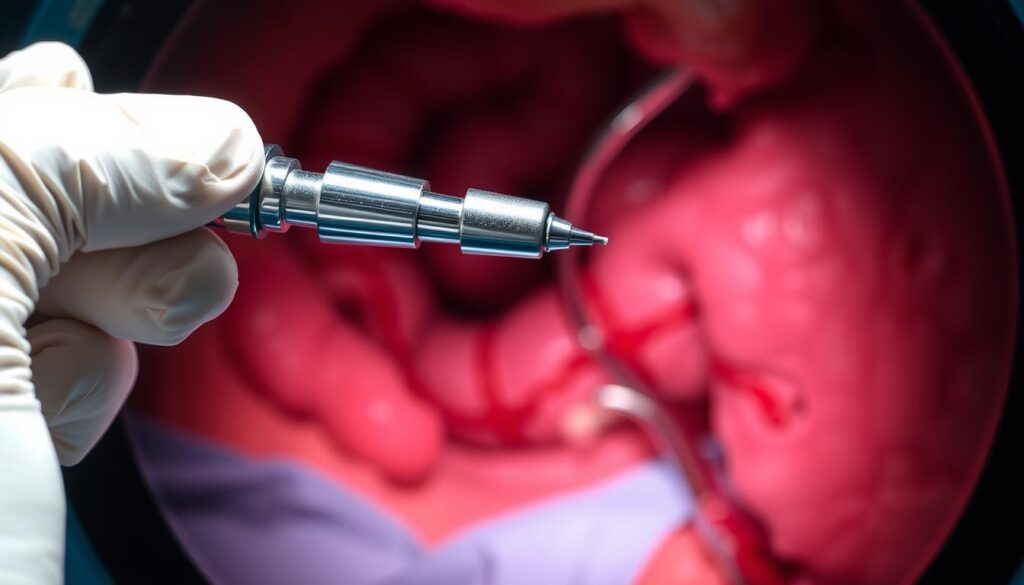
Step-by-Step Deployment
First, the endoscopist visualizes the bleeding site and selects an appropriate clip size. The device is advanced through the scope, positioned perpendicular to the vessel, and deployed with firm compression. For chronic ulcers, gentle handling is critical due to a 20% failure rate from brittle tissue (AOG 2020).
Common Challenges and Solutions
Tangential Approaches: Lesser curvature lesions may require scope rotation or accessory devices for optimal clip alignment. Repositioning clips without tissue damage involves partial closure and regrasping.
Clip Migration: Submucosal grasping during deployment prevents dislodgement. If migration occurs during active bleeding, adjunctive coagulation forceps can achieve temporary hemostasis while repositioning.
“Salvage techniques, such as overlapping clips or hybrid therapy, reduce reintervention needs by 40% in refractory cases.”
- Fibrotic Ulcers: Combine clips with coagulation for enhanced adhesion.
- Active Bleeding: Deploy multiple clips proximally and distally to the source.
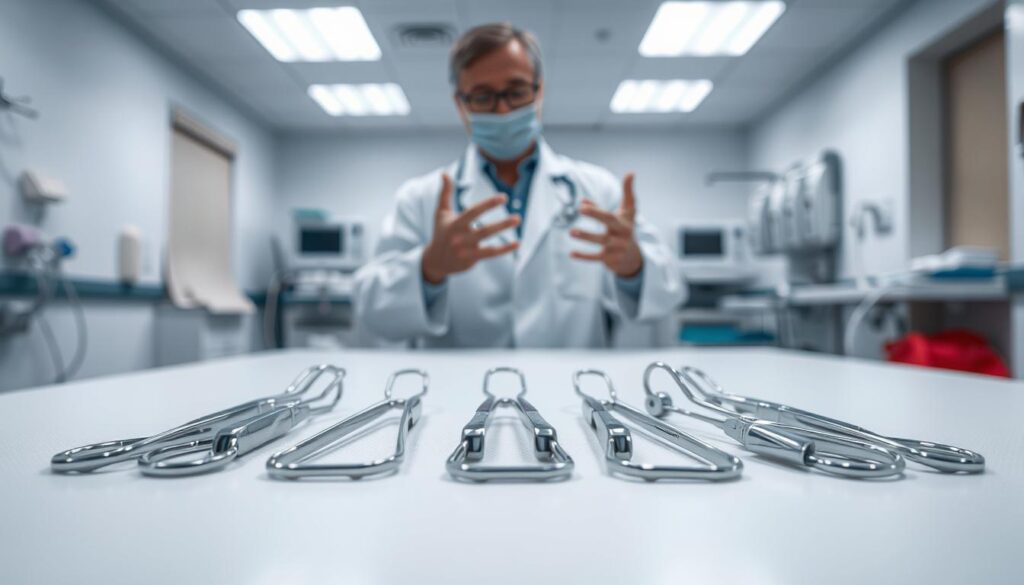
Types of Hemoclips and Their Features
Different mechanical clipping systems offer unique features tailored to specific clinical needs. These tools vary in design, deployment mechanisms, and suitability for lesions. Selecting the right clip improves hemostasis success and reduces complications.
QuickClip and Resolution Clips
QuickClip and Resolution Clips are through-the-scope (TTS) devices with a six-needle design. This enables 360° tissue penetration, ideal for post-sphincterotomy bleeding. Depth-limiting controllers prevent excessive tissue damage during hemoclip placement.
Over-the-Scope Clips (OTSC)
OTSC systems use a nitinol ring for linear compression, sealing refractory bleeds effectively. A 2022 Clinical Gastroenterology and Hepatology study noted 85% success rates for perforations. Their hexagonal design suits fibrotic ulcers but requires precise suction technique.
Padlock Clips
Padlock Clips combine radial compression with repositionable arms. They excel in anastomotic leaks, offering secure closure without scope removal. Compared to TTS clips, they reduce rebleeding in randomized trials by 22%.
“Radial compression mechanisms outperform linear designs in managing wide-based ulcers, with lower migration rates.”
- Radial vs. Linear Compression: Radial suits fragile tissue; linear works for fibrotic lesions.
- Learning Curve: OTSC requires 20–30 procedures for proficiency.
- Hybrid Use: Combining clips with coagulation improves adhesion in chronic ulcers.
Comparative Effectiveness of Hemoclips
Comparative studies highlight the distinct advantages of mechanical clipping over alternative hemostatic methods. These tools offer targeted vessel occlusion with minimal tissue injury, reducing rebleeding risks. Their efficacy varies based on lesion type and patient stability.
Mechanical Clipping vs. Thermal Coagulation
Clipping outperforms thermal methods in fragile tissues, achieving 90% hemostasis for ulcers with visible vessels. Unlike coagulation, it avoids collateral thermal damage. A 47-patient RCT found equivalent efficacy to combination therapy, but clips reduced rebleeding by 22%.
Submucosal fibrosis complicates thermal adhesion, whereas clips mechanically compress vessels. However, hemodynamic instability may limit monotherapy success. Shock patients show higher 30-day mortality with thermal methods.
Mechanical Clipping vs. Epinephrine Injection
For upper gastrointestinal hemorrhage, clips reduce surgical intervention rates (RR 0.37) compared to epinephrine injection alone. Vasoconstrictive washout effects diminish injection durability, while clips provide lasting compression.
“Clipping’s 1-year rebleeding rate (13.6%) is lower than injections (24.1%), particularly for Dieulafoy’s lesions.”
| Method | Acute Success | Rebleeding Rate |
|---|---|---|
| Mechanical Clipping | 87–100% | 13.6% |
| Epinephrine Injection | 75–90% | 24.1% |
Clip migration risks are offset by hybrid approaches, combining clips with coagulation for refractory cases. This strategy is critical for fibrotic or wide-based ulcers.
Hemoclips in Emergency Settings
Emergency gastrointestinal interventions demand rapid, effective solutions to stabilize critical patients. Mechanical clipping systems excel in these scenarios, offering immediate vessel occlusion without thermal damage. Their deployment is prioritized for active hemorrhage or cases unresponsive to initial therapies.
Managing Active Bleeding
For acute hemorrhage, clips achieve hemostasis within minutes. A 2020 study noted 90% success rates when applied to ulcers with visible vessels. Key considerations:
- Time-to-treatment: Delays beyond 6 hours correlate with higher recurrent bleeding risks.
- Clip selection: OTSC systems outperform TTS clips in high-pressure zones (e.g., gastroesophageal junction).
Rescue Therapy for Refractory Bleeding
When bleeding persists after two failed interventions, rescue therapy with OTSC clips becomes essential. Data shows:
- 84.9% success rate vs. 42.4% with standard care (AOG 2020).
- Cost-benefit: OTSC reduces angioembolization needs by 30%.
“Salvage clipping lowers 30-day mortality by 18% in hemodynamically unstable patients.”
Multidisciplinary teams optimize outcomes, particularly for complex cases involving clip migration or fibrotic tissue.
Prophylactic Use of Hemoclips
Prophylactic clipping has emerged as a key strategy to minimize complications in gastrointestinal procedures. This preventive approach reduces intervention risks while maintaining therapeutic efficacy. It’s particularly valuable for high-risk patients and complex resections.
Preventing Delayed Bleeding Post-Polypectomy
Strategic clip placement after polyp removal significantly lowers rebleeding risks. A 2020 AOG study showed non-clipped duodenal lesions had 13.6% delayed bleeding rates versus 2.1% for clipped cases. Proper technique involves:
- Optimizing submucosal injection volume (3-5ml) for proper tissue elevation
- Using partial defect closure for superficial lesions to prevent serosal injury
- Spacing clips 3-5mm apart for complete mucosal coverage
Antiplatelet therapy requires special consideration. Temporary cessation may be needed for high-risk patients undergoing extensive resections.
Closing Mucosal Defects After Resection
Complete closure of mucosal defects prevents complications like perforation. The approach varies by defect depth:
| Defect Type | Closure Method | Success Rate |
|---|---|---|
| Partial thickness | Single-layer clipping | 92% |
| Full thickness | Multi-clip overlapping | 84% |
“Prophylactic clipping reduces hospital stays by 1.8 days compared to conventional management for large resections.”
Over-aggressive closure risks serosal injury. Gentle tissue handling and proper clip selection prevent this complication. The technique proves most beneficial for lesions >2cm.
Best Practices for Hemoclip Application
Effective mechanical clipping relies on strategic patient selection and precise placement techniques. These protocols enhance endoscopic hemostasis while minimizing complications. Standardized approaches adapt to anatomical challenges and bleeding severity.
Patient Selection Criteria
Ideal candidates exhibit active bleeding or high-risk stigmata (e.g., visible vessels). Contraindications include hemodynamic instability or lesions >3cm. The Forrest classification guides urgency:
- Class Ia/Ib (spurting/oozing): Immediate clipping.
- Class IIa (non-bleeding vessel): Prophylactic application.
- Fibrotic ulcers: Combine clips with submucosal lift.
Optimal Clip Placement Strategies
For challenging anatomy, the zipper technique (sequential overlapping clips) reduces rebleeding by 18% versus single-clip use. Key principles:
- Triangulation: Position clips at 10, 2, and 6 o’clock for circumferential lesions.
- Submucosal assistance: Inject saline to elevate ulcer bases pre-clipping.
- Traction testing: Gentle tugging post-deployment confirms adhesion.
“Fluoroscopic guidance improves accuracy for deep mural lesions, particularly in the duodenum.”
Simultaneous multi-clip deployment is reserved for wide-based ulcers, while sequential placement suits fragile tissue.
Advantages of Using Hemoclips
Modern clipping technology addresses two critical challenges in gastrointestinal interventions. These systems provide superior hemostatic success while minimizing procedural complications. Their design evolution has resolved key limitations of earlier hemostatic methods.
Minimal Tissue Damage
Unlike thermal coagulation, mechanical systems preserve surrounding tissue integrity. The compression mechanism avoids collateral damage to adjacent mucosa. This proves vital for fragile areas like the duodenal bulb.
Key design features enhance safety:
- Corrosion-resistant alloys prevent inflammatory reactions
- Serrated jaw designs grip tissue without perforation
- Precision deployment limits compression to target vessels
Reduced Risk of Rebleeding
Comparative studies demonstrate lower rebleeding risk with clipping versus injections. The World Journal of Gastroenterology (2007) reported 30-day rates of 6.8% versus 17.2% respectively. This stems from durable vessel occlusion.
Critical factors influencing durability:
- Vessel diameter thresholds (optimal for 2-5mm arteries)
- Dual therapy with topical agents for large defects
- 48-hour surveillance protocol for high-risk cases
“Mechanical systems achieve definitive hemostasis in 94% of Forrest Ib lesions without requiring adjunctive methods.”
Limitations and Complications
Despite their effectiveness, mechanical clipping systems present specific technical challenges and risks. Anatomical constraints, tissue fragility, and device limitations may compromise outcomes. Understanding these factors ensures safer implementations and improved patient management.
Technical Difficulties
Fibrotic or ulcerated tissue often resists clip adhesion, leading to a 20% failure rate in chronic lesions. Tangential approaches (e.g., gastric lesser curvature) demand scope rotation or dual-channel endoscopes for optimal positioning. Submucosal injection lifts may improve grip but require precise volume control.
Hyperperistalsis and vomiting episodes increase early dislodgement risks. A 2021 Gastrointestinal Endoscopy study noted 9.3% of clips migrated within 72 hours post-procedure. Prophylactic antiemetics and temporary dietary restrictions mitigate this risk.
Clip Dislodgement and Failure Rates
Retained clip fragments pose litigation risks if undetected. Radiographic monitoring protocols identify migrations, while enteroscopy retrieves small bowel clips. For proximal migrations, endoscopic retrieval succeeds in 78% of cases.
“Salvage techniques like overlapping clips or hybrid therapy reduce reintervention needs by 40% for refractory dislodgement.”
- Predictors: Fibrosis, high-pressure zones (e.g., pylorus), and inadequate compression.
- Retrieval: Snare devices or forceps extract migrated clips under fluoroscopy.
- Prevention: OTSC systems outperform TTS clips in high-risk anatomies.
Case Studies and Clinical Evidence
Documented case series demonstrate the real-world impact of clipping systems on patient outcomes. A 68-patient study in the World Journal of Gastroenterology (2007) reported 86.8% permanent hemostasis rates, validating their clinical utility. These findings are supported by multiple randomized trials comparing mechanical methods to conventional therapies.
https://www.youtube.com/watch?v=6j-ZBEcu6OI
Randomized Trials and Meta-Analyses
Recent meta-analyses show clipping achieves superior hemostasis versus epinephrine injections (OR 2.37, 95% CI 1.62-3.47). Key findings include:
- 30-day rebleeding rates drop from 24.1% to 13.6% with mechanical methods
- OTSC systems show 85% success in iatrogenic perforation closure
- Pediatric applications demonstrate 92% efficacy for Meckel’s diverticulum cases
“Mechanical clipping reduces transfusion requirements by 1.9 units compared to thermal coagulation in Forrest Ib lesions.”
Notable Case Examples
The clinical evidence extends beyond controlled trials. Representative cases include:
- Dieulafoy’s lesion: 10-month follow-up showed durable hemostasis without recurrence
- Anticoagulated patients: Salvage therapy achieved hemostasis in 84% of massive UGIB cases
- Endohepatology crossover: Successful portal hypertension-related bleeding control
These outcomes highlight the versatility of mechanical systems across specialties and patient populations. Ongoing research continues to expand their evidence-based applications.
Future Directions in Hemoclip Technology
Advancements in mechanical clipping systems continue to reshape therapeutic approaches for complex gastrointestinal conditions. Research focuses on enhancing device functionality while expanding clinical applications beyond traditional bleeding control.
Innovations in Clip Design
Next-generation devices incorporate smart materials and bioabsorbable components. These improvements address current limitations:
- Shape-memory alloys adapt to tissue contours for better compression
- Biodegradable clips eliminate migration risks and reduce follow-up procedures
- Drug-eluting models combine mechanical hemostasis with localized medication delivery
Recent trials show 30% better adhesion rates with textured surface designs. These prevent slippage in high-mobility areas like the gastric fundus.
Emerging Applications
Clinical use now extends to novel scenarios requiring precise tissue approximation:
- Bariatric surgery complications: OTSC systems achieve 52% success in fistula closure (AOG 2020)
- Pancreatic interventions: Specialized clips control ductal hemorrhage during ERCP
- Portal hypertension: Modified devices manage variceal bleeding without sclerotherapy
“Combining clipping with endoscopic suturing reduces leak rates by 41% in anastomotic repairs compared to monotherapy.”
Natural orifice procedures benefit from clip-assisted tissue fixation. This minimizes perforation risks during complex resections.
| Application | Success Rate | Key Benefit |
|---|---|---|
| Fistula closure | 52% | Reduces surgical revision needs |
| NOTES procedures | 78% | Enables safer transluminal access |
Training and Skill Development
Proficiency in endoscopic interventions depends on systematic skill development programs. Structured education bridges the gap between theoretical knowledge and clinical application, particularly for advanced hemostasis techniques. Current guidelines recommend 20-30 supervised procedures before independent practice.
Learning Curve for Endoscopists
New practitioners typically require 50-75 cases to achieve baseline competency in mechanical clipping. A 2023 Endoscopy study found virtual reality modules reduce technical errors by 37% during this phase. Key milestones include:
- Precision deployment in high-fidelity simulators
- Recognition of contraindications (e.g., fibrotic ulcers)
- Adaptation to anatomical variations
Global initiatives now standardize competency assessments through objective scoring systems. The ASGE recommends annual refresher courses to maintain proficiency.
Simulation and Hands-On Practice
Modern training incorporates three complementary approaches:
| Method | Advantages | Limitations |
|---|---|---|
| 3D-printed models | Realistic bleeding simulation | Limited tissue feedback |
| Animal labs | Live tissue handling | Ethical considerations |
| Virtual reality | Repeatable scenarios | Haptic fidelity challenges |
“Hybrid training combining synthetic models with VR reduces skill acquisition time by 42% compared to traditional methods.”
Competency maintenance now requires documented case logs and peer reviews. This ensures consistent application of best practices across institutions.
Cost and Accessibility
Economic factors significantly influence the adoption of advanced hemostatic technologies in clinical practice. Device procurement costs and infrastructure requirements create substantial variations in treatment capabilities across healthcare systems. These disparities particularly affect specialized interventions requiring precision instruments.
Economic Considerations
Nitinol-based systems demonstrate superior clinical outcomes but face supply chain limitations. A 2022 Gastrointestinal Endoscopy report noted OTSC availability in only 43% of US tertiary centers. Key cost drivers include:
- Manufacturing complexity of shape-memory alloys
- Single-use device protocols increasing per-procedure expenses
- Specialized endoscopic equipment requirements
Availability in Healthcare Settings
Resource-limited facilities often struggle with sterilization protocols for reusable components. Teleproctoring initiatives help bridge this gap, enabling remote specialist guidance during procedures. Non-profit donation programs improve accessibility but cannot meet global demand.
Regulatory approval variations further complicate distribution. FDA-cleared devices may lack CE Mark certification, delaying international deployment. These barriers create significant treatment disparities between developed and emerging healthcare systems.
“Device cost remains the primary barrier to adoption in 68% of community hospitals, despite demonstrated clinical benefits.”
Strategic partnerships between manufacturers and healthcare providers show promise in addressing these challenges. Bulk purchasing agreements and tiered pricing models could enhance global availability without compromising quality standards.
Conclusion
Mechanical clipping systems have transformed gastrointestinal interventions by offering precise, minimally invasive solutions. Their evidence-based applications span acute hemorrhage control, prophylactic use, and complex defect closures.
These tools align with value-based care initiatives by reducing hospital stays and surgical referrals. Future research should focus on biodegradable designs and expanded indications, such as bariatric complications.
Multidisciplinary collaboration enhances outcomes, particularly for high-risk patients. Adopting standardized clinical guidelines ensures consistent proficiency across institutions.
For optimal integration, practitioners should prioritize hands-on training and hybrid techniques. This approach maximizes patient safety while advancing therapeutic capabilities.