Noncancerous growths along the digestive tract’s mucosal lining are frequently identified during routine screenings. These lesions, often categorized by their shape and location, are typically detected through colonoscopy procedures. While most demonstrate benign behavior, variations in size and morphology influence clinical management strategies.
Current literature highlights two primary morphological classifications: pedunculated and sessile. The latter, characterized by a flat base, accounts for approximately 70% of cases in the colon and rectum. Distribution patterns show higher prevalence in distal colonic segments compared to proximal regions.
Though malignant transformation remains uncommon, specific risk indicators warrant attention. Lesions exceeding 10mm in diameter or appearing in clusters (polyposis) require thorough histological evaluation. Recent studies suggest a potential association between advanced cellular architecture and neoplastic progression.
This article examines diagnostic protocols, histological features, and evidence-based surveillance guidelines. Subsequent sections will analyze risk stratification models and contemporary excision techniques for healthcare practitioners.
Key Takeaways
- Common noncancerous growths in the colon and rectal lining
- Typically identified during preventive colonoscopy screenings
- Morphological variations include sessile and pedunculated forms
- Size and quantity influence clinical risk assessment
- Requires differential diagnosis from malignant lesions
- Pathology reports guide treatment decision-making
Overview of Hyperplastic Polyps
Benign mucosal growths in the gastrointestinal tract present distinct histological patterns that differentiate them from neoplastic counterparts. These formations primarily consist of elongated crypts with characteristic serrations, visible under microscopic examination. Their typical size ranges from 1-5mm, though larger specimens occasionally occur in distal colonic regions.
Definition and Characteristics of Polyps
Histopathological analysis reveals non-dysplastic epithelial cells arranged in a sawtooth configuration, a hallmark feature. Unlike adenomas, these growths maintain normal nuclear polarity and lack significant mitotic activity. Mucin-rich cytoplasm and stromal inflammation frequently accompany these architectural changes.
Types and Locations in the Colon and Stomach
Two primary morphological categories dominate clinical observations:
| Type | Morphology | Common Locations | Histological Features |
|---|---|---|---|
| Sessile | Flat base | Rectosigmoid colon | Star-shaped crypts |
| Pedunculated | Stalk-like structure | Transverse colon | Elongated glands |
| Traditional Serrated | Leaf-like projections | Gastric antrum | Eosinophilic cells |
Gastric variants demonstrate different cellular architecture compared to colonic forms, often requiring immunohistochemical staining for accurate classification. Distal colorectal segments host approximately 80% of cases, while proximal regions account for less than 15%.
Diagnosis and Follow-Up Procedures
Modern diagnostic approaches combine endoscopic visualization with histological analysis to assess mucosal abnormalities. Gastroenterologists prioritize colonoscopy as the gold standard for identifying growths in the colon, enabling direct visualization and tissue sampling. Advanced imaging enhancements like narrow-band imaging improve detection rates for flat lesions, particularly in the rectosigmoid region.
Role of Colonoscopy and Biopsy Techniques
During the procedure, suspicious areas undergo targeted biopsy using cold forceps or snare techniques. Specimens are analyzed for architectural patterns, including crypt serration and cellular dysplasia. Sessile serrated polyps require careful examination due to their subtle mucosal changes and potential association with cancer risk.
Interpreting Your Pathology Report
Histopathological findings determine clinical management. Reports typically classify lesions as hyperplastic, adenomatous, or serrated. Key indicators include:
- Presence of dysplastic cells in adenomas
- Crypt branching patterns in serrated variants
- Margin status for completely excised lesions
Patients with multiple growths or polyposis syndrome require tailored surveillance plans. Current guidelines recommend repeat colonoscopy within 3-5 years for high-risk findings, while isolated benign lesions may need extended intervals.
Risk Factors and Preventive Measures
Multiple modifiable and non-modifiable factors influence colorectal mucosal lesion development. Epidemiological studies associate high body mass index with a 40% increased incidence of distal colon abnormalities. Diets rich in processed meats and saturated fats demonstrate stronger correlations than genetic predisposition alone.
Key risk enhancers include chronic inflammatory bowel diseases and prolonged tobacco use. Alcohol consumption exceeding 30g daily elevates rectal lesion risks by altering mucosal repair mechanisms. First-degree relatives of patients with colorectal malignancies show threefold higher detection rates during screening.
| Risk Factor | Impact Level | Preventive Countermeasure |
|---|---|---|
| High Red Meat Intake | Moderate | Plant-based diet adoption |
| Smoking >10 pack-years | High | Smoking cessation programs |
| BMI >30 kg/m² | Significant | Structured weight management |
| Family History Positive | Elevated | Early surveillance colonoscopy |
Clinical trials indicate regular NSAID use reduces cancer progression risks by 25-30% through COX-2 inhibition. Calcium supplementation (1200mg daily) demonstrates protective effects against cellular hyperproliferation in the large intestine.
Current guidelines recommend initial screening at age 45 for average-risk populations. Patients with multiple growths or polyposis syndromes require personalized monitoring intervals based on histological findings and familial patterns.
Effective Treatment Strategies for hyperplastic polyp
Clinical management of colorectal mucosal growths prioritizes risk reduction and lesion eradication. Treatment plans depend on lesion size, quantity, and histological features identified during endoscopic evaluation. Most small formations require minimal intervention, while complex cases demand specialized approaches.
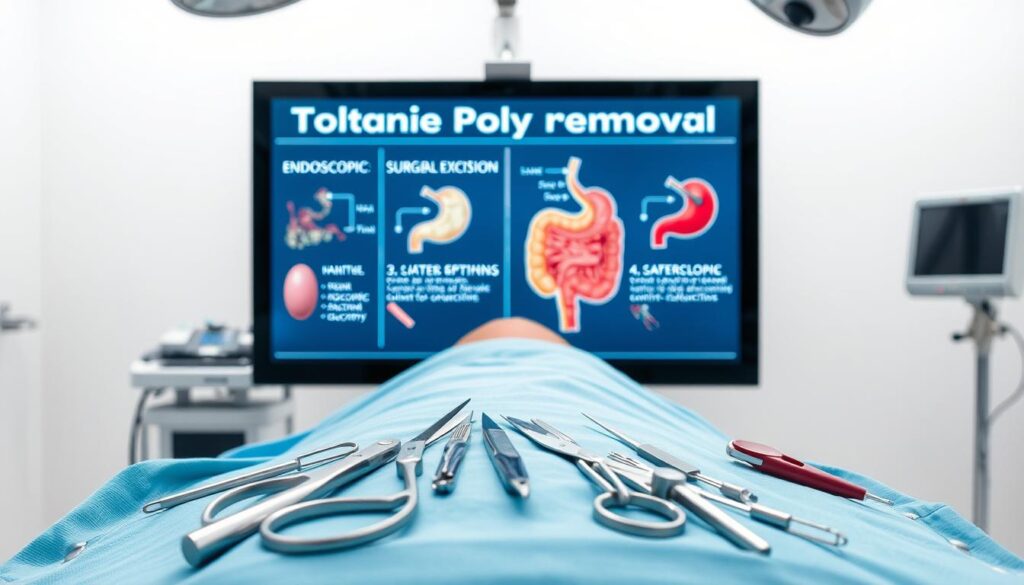
Non-Invasive Removal and Monitoring Methods
Endoscopic polypectomy remains the primary intervention for lesions under 10mm. Gastroenterologists use cold snares or biopsy forceps during routine colonoscopy to excise growths. Larger specimens may require electrocautery devices to prevent bleeding.
Follow-up intervals align with pathology findings. Isolated benign growths typically need repeat colonoscopy in 7-10 years. Patients with multiple lesions or sessile serrated features require 3-year surveillance cycles.
Surgical and Advanced Intervention Options
Complex cases involving clustered growths or suspicious cellular changes often warrant surgical consultation. Advanced techniques like endoscopic mucosal resection (EMR) address flat lesions exceeding 20mm. Submucosal injection techniques enhance safety during tissue removal.
| Procedure | Indication | Recovery Time |
|---|---|---|
| Cold Snare Polypectomy | Lesions <10mm | 24-48 hours |
| EMR | Large flat growths | 3-5 days |
| Surgical Resection | Polyposis syndromes | 2-4 weeks |
Current guidelines emphasize complete excision margins to minimize recurrence risks. Pathological confirmation of benign status guides subsequent monitoring protocols. High-risk patients receive tailored plans addressing familial cancer patterns and comorbidities.
Conclusion
Comprehensive colorectal care integrates diagnostic insights with preventive strategies to manage mucosal abnormalities effectively. Most growths identified during screenings demonstrate benign behavior, particularly when detected early. Differentiation from adenomas remains essential due to their distinct cellular profiles and cancer risk potential.
Patients with family history or polyposis syndromes require tailored surveillance plans aligned with current guidelines. Regular colonoscopies and risk factor modification, such as dietary adjustments, reduce complications. Emerging research enhances stratification models, particularly for lesions in distal colon regions.
Clinical vigilance through multidisciplinary approaches ensures optimal outcomes. While progression to malignancy remains rare, adherence to excision protocols and follow-up intervals maintains safety. Ongoing studies focus on molecular markers to refine personalized management, reinforcing evidence-based standards in gastrointestinal health.