Endoscopic mucosal resection (EMR) has become a cornerstone in the management of colorectal polyps. Recent studies have provided valuable insights into the efficacy and safety of different techniques. The German CHRONICLE Trial (2024) compared methods for large nonpedunculated colorectal polyps, involving 764-777 patients. This trial, along with a 13-study meta-analysis (2023) evaluating 1,896 serrated polyps, offers a comprehensive view of outcomes.
A Korean RCT (2024) further examined techniques for smaller polyps, analyzing 138 lesions. These studies highlight the importance of selecting the appropriate method based on polyp size. For instance, a 2024 Gastroenterology study reported a 98.6% en-bloc resection rate with one technique, while the meta-analysis noted residual polyp rates of 4.5% vs. 5.1%.
Understanding these findings is crucial for optimizing patient outcomes. The data underscores the need for tailored approaches in clinical practice. This section delves into the key trials and their implications for endoscopic procedures.
Key Takeaways
- The German CHRONICLE Trial compared techniques for large colorectal polyps.
- A meta-analysis evaluated 1,896 serrated polyps across 13 studies.
- The Korean RCT focused on smaller polyps, analyzing 138 lesions.
- Polyp size significantly influences the choice of resection technique.
- Recent studies highlight high en-bloc resection rates and residual polyp risks.
Introduction to Cold Versus Hot EMR
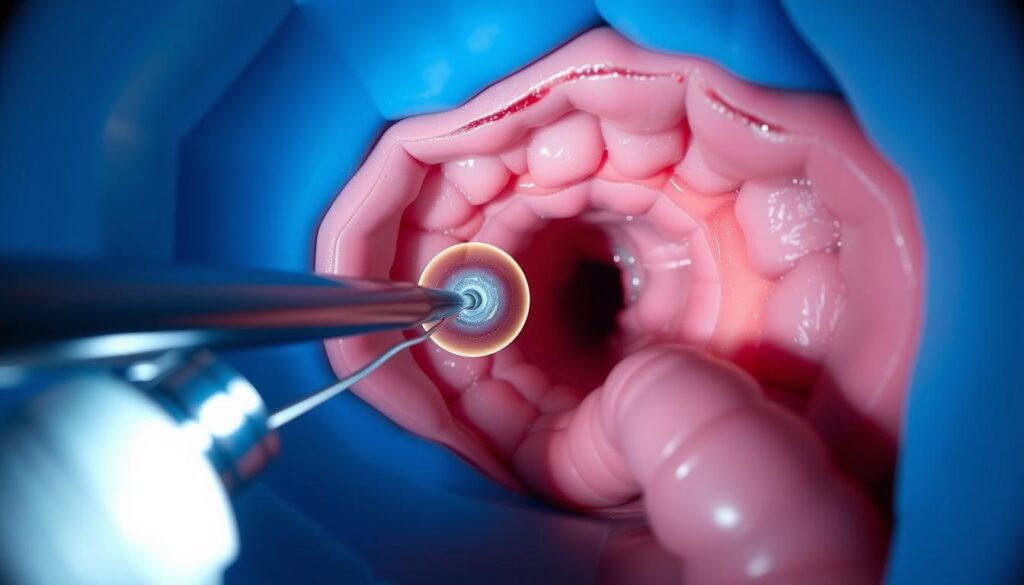
The removal of mucosal lesions through endoscopic techniques has revolutionized gastrointestinal treatment. Endoscopic mucosal resection (EMR) is a minimally invasive procedure designed to treat precancerous and early-stage lesions. It involves the removal of abnormal tissue from the mucosal layer, often with the aid of submucosal injection to ensure safety and precision.
EMR is categorized into two primary techniques: cold and hot. The cold technique uses mechanical transection without electrocautery, while the hot technique employs electrosurgical current for tissue removal. Both methods have distinct mechanisms and applications, making them suitable for different clinical scenarios.
What is Endoscopic Mucosal Resection (EMR)?
Endoscopic mucosal resection is defined as the resection of mucosal lesions with submucosal injection. This procedure is often the first-line treatment for non-invasive neoplasia removal. It allows for precise tissue excision while minimizing damage to surrounding healthy tissue.
Submucosal injection protocols typically involve a mixture of normal saline and indigo carmine. This solution helps lift the lesion, creating a safety cushion and improving visibility during the procedure. The use of specialized snares, such as 10-15mm oval snares, ensures accurate and efficient tissue removal.
Overview of Cold and Hot EMR Techniques
The choice between cold and hot techniques depends on the lesion’s characteristics and the clinician’s expertise. The cold method is preferred for smaller lesions due to its simplicity and reduced risk of thermal injury. In contrast, the hot technique is often used for larger lesions, leveraging electrosurgical current for effective tissue removal.
| Aspect | Cold Technique | Hot Technique |
|---|---|---|
| Mechanism | Mechanical transection | Electrosurgical current |
| Procedural Time | 172 seconds (median) | 186 seconds (median) |
| Thermal Injury Risk | Low | Moderate |
Understanding these techniques and their applications is essential for optimizing patient outcomes. Clinicians must consider factors such as lesion size, location, and procedural time when selecting the appropriate method.
Techniques Compared: Cold EMR vs. Hot EMR
The evolution of endoscopic techniques has introduced distinct methods for polyp removal. Each approach offers unique advantages, tailored to specific clinical scenarios. This section explores the procedural details and methodologies of cold snare and hot snare techniques.
Cold EMR: Procedure and Methodology
The cold snare technique involves mechanical transection without the use of electrocautery. This method is particularly effective for smaller lesions. The procedure begins with a submucosal injection to lift the lesion, ensuring a clear margin of 2mm for snaring.
Margin assessment is often enhanced using narrow-band imaging (NBI) or magnification. This step ensures precise tissue removal and minimizes the risk of residual polyps. However, specimen fragmentation is more common with this technique, which can complicate histological evaluation.
Studies indicate an R0 resection rate of 55.7% for the cold method. Performance variations are notable between trainees and experts, with experienced clinicians achieving higher success rates.
Hot EMR: Procedure and Methodology
The hot snare technique employs electrosurgical current for tissue removal. This method is often preferred for larger lesions due to its efficiency. The VIO300D generator is commonly used, with settings adjusted for forced coagulation.
Electrosurgical settings are carefully calibrated to balance tissue removal and thermal injury risk. This approach achieves an R0 resection rate of 82.4%, significantly higher than the cold method. En-bloc rates are comparable, with 98.5% success in recent trials.
Performance differences between trainees and experts are less pronounced with the hot technique. This is attributed to the standardized nature of electrosurgical settings.
| Aspect | Cold Snare | Hot Snare |
|---|---|---|
| Mechanism | Mechanical transection | Electrosurgical current |
| R0 Resection Rate | 55.7% | 82.4% |
| Specimen Fragmentation | Common | Rare |
Efficacy of Cold Versus Hot EMR
The effectiveness of endoscopic techniques in polyp removal has been a focal point in recent clinical studies. A key aspect of these studies is the comparison of residual polyp rates and en-bloc resection rates. These metrics provide critical insights into the success of different methods.
Residual Polyp Rates
Pooled data from a meta-analysis revealed residual polyp rates of 4.5% for the cold technique and 5.1% for the hot technique (P=0.9). This suggests minimal difference in incomplete resection between the two methods. However, the high piecemeal rate of 99.3% in cold techniques compared to 59.2% in hot techniques (P
Piecemeal resection, while effective in removing larger lesions, can complicate histological assessment. This underscores the importance of achieving R0 resection for accurate diagnosis and treatment planning.
En-bloc Resection Rates
The en-bloc resection rate for cold techniques was significantly lower at 1.4%, compared to 41.4% for hot techniques (P
In a Korean study, 6-month residual recurrence rates were 0% for cold techniques and 1.5% for hot techniques. These findings suggest that while cold techniques may reduce immediate recurrence, they require careful follow-up to ensure long-term success.
| Aspect | Cold Technique | Hot Technique |
|---|---|---|
| Residual Polyp Rate | 4.5% | 5.1% |
| Piecemeal Rate | 99.3% | 59.2% |
| En-bloc Resection Rate | 1.4% | 41.4% |
These findings highlight the need for tailored approaches based on lesion characteristics. Clinicians must weigh the benefits of each technique against potential limitations to optimize patient outcomes.
Safety Profiles: Cold vs. Hot EMR
Understanding the safety profiles of endoscopic techniques is critical for minimizing adverse events. This section examines the risks associated with different methods, focusing on bleeding and perforation.
Immediate and Delayed Bleeding Risks
Bleeding is a common concern in endoscopic procedures. Immediate bleeding occurs in 11.4% of cases with the cold technique, compared to 7.4% with the hot technique. Delayed bleeding is less frequent but more significant, with rates of 0.7% for cold and 4% for hot methods (P=0.05).
In pedunculated polyps, 75% of cases using the cold technique involve bleeding risks. Endoscopic closure protocols, such as clipping visible vessels, are essential to mitigate these risks. Hemodialysis patients are particularly susceptible due to impaired coagulation.
Perforation Risks
Perforation is a rare but serious complication. A meta-analysis of 1,896 serrated polyps reported no perforations in either technique. This highlights the overall safety of both methods when performed by skilled clinicians.
Median procedure times are 172 seconds for cold and 186 seconds for hot techniques. Longer procedural times may increase the risk of complications, emphasizing the need for efficiency.
- Delayed bleeding: 0.7% cold vs. 4% hot (P=0.05).
- Immediate bleeding: 11.4% cold vs. 7.4% hot.
- No perforations in 1,896 serrated polyps.
- Endoscopic closure protocols reduce bleeding risks.
- Hemodialysis patients require careful monitoring.
Post-polypectomy syndrome, though rare, is another consideration. Clinicians must balance procedural efficiency with safety to optimize outcomes for patients.
Clinical Outcomes of Cold and Hot EMR
Long-term clinical outcomes are critical for evaluating the success of endoscopic procedures. Recent studies have provided valuable data on follow-up results, recovery rates, and complications. These insights help refine clinical practices and improve patient care.
Long-term Follow-up Results
A meta-analysis with a 15.3-month median follow-up revealed durable results for both techniques. Maximum follow-up durability was evaluated at 37 months, showing consistent efficacy. Surveillance colonoscopy protocols, such as the 6-month interval in a Korean RCT, ensured thorough monitoring of lesions.
Scar assessment techniques, including narrow-band imaging, were employed to detect residual tissue. These methods enhance the accuracy of follow-up evaluations and reduce recurrence risks. Lost-to-follow-up rates were minimal, with only two patients in the RCT not completing the study.
Patient Recovery and Complication Rates
Delayed bleeding rates were 2.9% for one technique and 1.5% for the other at 14 days. Outpatient complication monitoring protocols were implemented to track adverse events. Histopathological review processes ensured accurate diagnosis and treatment planning.
Post-procedure recovery was closely monitored, with emphasis on minimizing complications. The findings highlight the importance of tailored follow-up strategies to optimize outcomes.
| Aspect | Technique A | Technique B |
|---|---|---|
| Median Follow-up | 15.3 months | 15.3 months |
| Delayed Bleeding | 2.9% | 1.5% |
| Lost-to-Follow-up | 2 patients | 2 patients |
Cold EMR for Small Colorectal Polyps
The management of small colorectal polyps has seen significant advancements with the introduction of specialized techniques. Among these, cold snare polypectomy has emerged as a preferred method for lesions under 10mm. This approach minimizes thermal injury and simplifies the procedure, making it ideal for smaller polyps.
Efficacy and Safety in Small Polyps
Studies have demonstrated a 55.7% R0 resection rate for cold snare polypectomy, compared to 82.4% for hot techniques. Despite the lower R0 rate, the technical success rate remains high at 98.6%. This highlights the method’s reliability for smaller lesions.
Residual recurrence rates for 6-9mm polyps were 0% with cold techniques, compared to 1.5% with hot methods. This suggests that cold techniques may reduce immediate recurrence risks. However, careful follow-up is essential to ensure long-term success.
Comparison with Hot EMR for Small Polyps
When comparing techniques, cold snare polypectomy shows a 40% Rx resection rate, while hot methods achieve 13.2%. This disparity underscores the importance of technique selection based on polyp characteristics.
Trainee performance also impacts outcomes, with one residual recurrence case reported in studies. Proper training and supervision are crucial to maintaining high standards. Additionally, submucosal injection enhances margin visualization, improving procedural accuracy.
- Median polyp size: 7mm.
- Rx resection rate: 40% cold vs. 13.2% hot.
- Trainee performance: 1 residual recurrence case.
- Pedunculated polyp management: challenges addressed.
- Submucosal injection: improves margin visualization.
Hot EMR for Large Nonpedunculated Polyps
The management of large nonpedunculated colorectal polyps presents unique challenges in endoscopic practice. These lesions, often flat or sessile, require precise techniques to ensure complete removal. Hot EMR has emerged as a preferred method for such cases, leveraging electrosurgical current for effective tissue resection.
Recent studies, including the CHRONICLE Trial, have provided valuable insights into the efficacy of this approach. The trial involved 764-777 patients with large polyps, demonstrating the technique’s reliability in complex scenarios.
Effectiveness in Large Polyps
For lesions up to 33mm, hot EMR achieves an en-bloc resection rate of 41.4%, significantly higher than cold techniques. This method is particularly effective for fibrotic tissue, where electrosurgical current ensures thorough removal. Piecemeal resection is often necessary for larger lesions, ensuring complete excision while minimizing risks.
Delayed bleeding rates are slightly higher with hot EMR, at 4%, compared to 0.7% for cold techniques. However, the benefits of complete resection often outweigh this risk, especially for serrated lesions. Proper endoscopic closure protocols, such as clipping visible vessels, further mitigate complications.
Risks and Benefits Compared to Cold EMR
While hot EMR offers higher en-bloc resection rates, it carries a greater risk of thermal injury. Immediate bleeding occurs in 7.4% of cases, compared to 11.4% with cold techniques. However, the method’s efficiency in removing large, flat polyps makes it indispensable in clinical practice.
| Aspect | Hot EMR | Cold EMR |
|---|---|---|
| En-bloc Resection Rate | 41.4% | 1.4% |
| Delayed Bleeding | 4% | 0.7% |
| Thermal Injury Risk | Moderate | Low |
Clinicians must weigh these factors when selecting the appropriate technique. For large nonpedunculated colorectal polyps, hot EMR remains a cornerstone of effective endoscopic management.
Systematic Review and Meta-Analysis Findings
Recent advancements in endoscopic research have highlighted the importance of systematic review meta-analysis in evaluating clinical outcomes. These studies provide a comprehensive understanding of efficacy and safety by integrating pooled data from multiple sources. This section delves into key findings and their implications for endoscopic practice.
Pooled Data on Efficacy and Safety
A systematic review meta-analysis of 13 studies analyzed 1,452 serrated sessile polyps (SSPs). The mean polyp size was 23.7mm, ranging from 15.9mm to 33mm. Heterogeneity in residual rate analysis was significant, with an I² value of 76%.
The random-effects model was employed to account for variability across studies. This approach ensures robust analysis by weighting studies based on sample size and quality. Funnel plots were used to assess publication bias, revealing minimal asymmetry and supporting the reliability of the findings.
Comparative Analysis of Techniques
Comparative analysis revealed notable differences between Asian and Western study populations. Asian studies reported higher en-bloc resection rates, while Western studies emphasized safety profiles. These variations highlight the need for context-specific guidelines.
Limitations in R0 resection reporting were identified, with inconsistencies in documentation across studies. The GRADE evidence quality assessment rated the overall evidence as moderate, underscoring the need for standardized reporting protocols.
- Mean polyp size: 23.7mm (range 15.9-33mm).
- Heterogeneity: I²=76% in residual rate analysis.
- Random-effects model: accounts for study variability.
- Publication bias: minimal asymmetry in funnel plots.
- GRADE assessment: moderate evidence quality.
These findings provide valuable insights for clinicians, emphasizing the importance of tailored approaches based on pooled data and regional variations.
Randomized Controlled Trials: Insights
Randomized controlled trials (RCTs) have significantly shaped modern endoscopic practices. These studies provide robust evidence to guide clinical decisions and improve patient outcomes. Recent trials, such as the CHRONICLE Trial and a Korean RCT, have offered valuable insights into the efficacy and safety of endoscopic techniques.
Key Findings from Recent Trials
The CHRONICLE Trial, a German multicenter RCT, involved 764-777 patients with large nonpedunculated colorectal polyps. This study compared endoscopic techniques, focusing on en-bloc resection rates and procedural safety. The results demonstrated overlapping 95% confidence intervals in primary outcomes, indicating comparable efficacy between methods.
In the Korean RCT, 99 patients with 138 polyps were analyzed. The study highlighted the importance of non-inferiority margins, with a 5% delta considered acceptable. Both trials adhered to CONSORT guidelines, ensuring transparency and methodological rigor in their designs.
Operator expertise played a significant role in outcomes. Expert operators achieved higher success rates compared to trainees, emphasizing the need for proper training and supervision. Intention-to-treat and per-protocol analyses were employed to validate the results, ensuring robust conclusions.
Implications for Clinical Practice
The findings from these RCTs have direct implications for clinical practice. Clinicians can use the data to select the most effective techniques based on polyp characteristics and patient profiles. The trials also underscore the importance of standardized protocols to minimize risks and improve results.
Sample size calculation methodologies were critical in these studies. Adequate participant numbers ensured statistical power, enabling reliable conclusions. These insights help refine endoscopic practices and enhance patient care.
| Aspect | CHRONICLE Trial | Korean RCT |
|---|---|---|
| Participants | 764-777 patients | 99 patients |
| Polyps Analyzed | Large nonpedunculated | 138 polyps |
| Non-inferiority Margin | 5% delta | 5% delta |
| CONSORT Adherence | Yes | Yes |
These trials highlight the value of RCTs in advancing endoscopic techniques. By integrating these findings into clinical practice, healthcare providers can optimize outcomes and reduce risks for their patients.
Choosing the Right Technique: Factors to Consider
Selecting the appropriate endoscopic technique requires careful evaluation of multiple factors. Both patient-specific considerations and polyp characteristics play a critical role in determining the optimal approach. Clinicians must balance efficacy, safety, and procedural complexity to achieve the best outcomes.
Patient-Specific Considerations
Patient factors significantly influence the choice of endoscopic resection. For instance, the exclusion of anticoagulant use in the Korean RCT highlights the importance of managing bleeding risks. Comorbidities, such as chronic kidney disease (CKD), also require special attention due to their impact on procedural safety.
Location-specific challenges further complicate decision-making. A study found that 64.3% of polyps were located in the right colon, an area known for its anatomical complexity. These factors underscore the need for individualized treatment plans tailored to each patient’s unique profile.
Polyp Characteristics and Technique Suitability
The morphology and size of lesions are critical determinants of technique suitability. Flat polyps, which accounted for 62.9% of cases in recent studies, often require more advanced resection methods. The Paris classification system provides a useful framework for evaluating lesion morphology and guiding treatment decisions.
Comparative analysis of sessile versus pedunculated lesions reveals distinct management strategies. Sessile lesions, for example, often necessitate piecemeal resection, while pedunculated lesions may be removed en-bloc. Surveillance interval recommendations also vary based on lesion characteristics, ensuring thorough follow-up.
| Factor | Consideration |
|---|---|
| Patient Comorbidities | Chronic kidney disease, anticoagulant use |
| Polyp Location | 64.3% right-colon distribution |
| Lesion Morphology | 62.9% flat polyps |
| Resection Technique | Piecemeal vs. en-bloc |
- Analyze comorbidity considerations (e.g., CKD).
- Discuss location-specific challenges (right colon).
- Evaluate Paris classification implications.
- Compare sessile vs. pedunculated lesion management.
- Address surveillance interval recommendations.
“Tailoring endoscopic techniques to individual patient and lesion profiles is essential for optimizing outcomes.”
Conclusion
Recent studies highlight the importance of selecting the appropriate endoscopic technique based on polyp size and characteristics. For small lesions, cold snare methods demonstrate non-inferiority, offering simplicity and reduced thermal injury risks. In contrast, hot techniques excel in achieving higher en-bloc resection rates for larger, more complex polyps.
Delayed bleeding risks vary between techniques, with hot methods showing slightly higher rates. Operator experience remains a critical factor in achieving optimal outcomes, particularly for trainees. Future research should focus on randomized controlled trials for lesions exceeding 40mm to further refine clinical guidelines.
By tailoring techniques to specific lesion profiles, clinicians can enhance efficacy and safety, ensuring better patient outcomes in endoscopic practice.