Key Takeaways
- Introduction to Endoscopy Techniques
- Medical Applications and Procedures
- How to describe the difference between rigid endoscopy and flexible endoscopy
- Advantages, Disadvantages, and Patient Outcomes
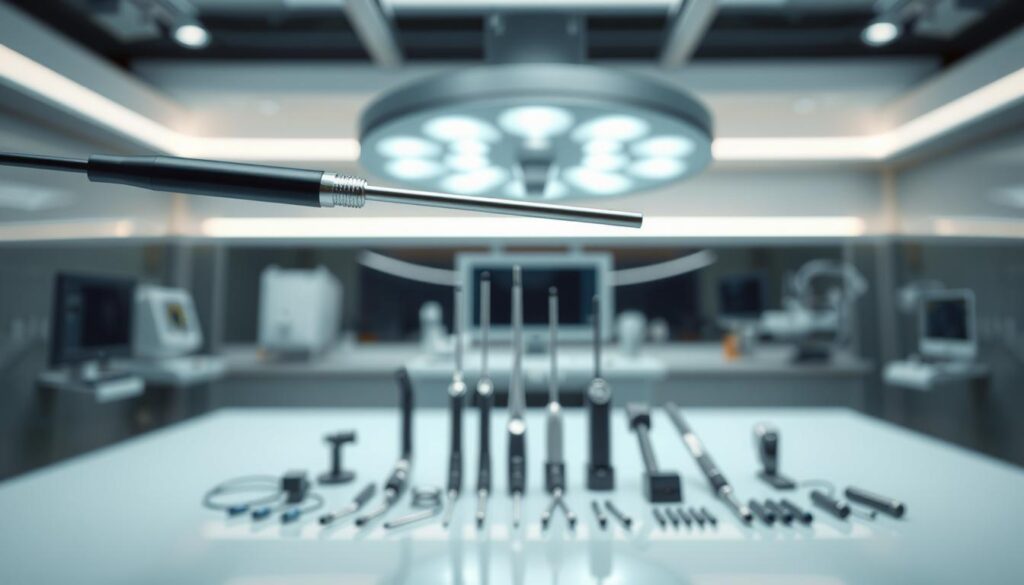
Modern medical practice relies heavily on endoscopic systems for diagnostic evaluations and therapeutic interventions. These instruments allow clinicians to examine internal structures through natural orifices or small incisions, minimizing patient trauma. The structural design of endoscopic tools significantly influences their clinical applications.
Rigid endoscopic devices feature a straight, non-bendable construction optimized for direct visualization in accessible anatomical regions. Their rigid architecture provides superior image resolution and stability during procedures requiring precise instrument control. These characteristics make them particularly suitable for orthopedic examinations and urological interventions.
Flexible endoscopic systems utilize pliable materials that navigate complex anatomical pathways. This adaptability enables access to convoluted structures within gastrointestinal or respiratory tracts. Advanced fiberoptic technology in these instruments maintains diagnostic accuracy while accommodating anatomical variations.
Key Takeaways
- Endoscopic systems are categorized by structural rigidity, influencing their clinical applications
- Rigid devices excel in procedures requiring stable visualization of accessible anatomy
- Flexible instruments navigate curved pathways in gastrointestinal and pulmonary systems
- Selection depends on target anatomy, procedural complexity, and required precision
- Both types incorporate advanced imaging technologies for accurate diagnostics
- Instrument choice directly impacts procedural success and patient outcomes
Introduction to Endoscopy Techniques
Clinical diagnostics have been transformed by endoscopic examination methods that combine optical precision with minimally invasive access. These medical devices enable detailed assessment of internal structures while reducing procedural risks compared to traditional surgical approaches.
What is Endoscopy?
Endoscopic procedures utilize specialized endoscopes to visualize anatomical regions through natural openings or minor incisions. Two primary variants exist:
- Rigid systems employ straight telescopic tubes with integrated cameras, ideal for direct visualization in accessible areas like joints or urinary tracts
- Flexible instruments navigate curved pathways using fiber-optic bundles, transmitting real-time images from the distal tip to external monitors
Both types incorporate imaging technology that converts optical data into electronic signals, enabling documentation and collaborative analysis during examinations.
Historical and Clinical Context
Early 19th-century prototypes evolved into modern digital platforms through advancements in optics and video processing. Today’s endoscopes support diverse applications:
- Gastrointestinal evaluations without surgical intervention
- Biopsy collection through integrated instrument channels
- Therapeutic interventions in pulmonary and urological fields
This technological progression has established endoscopic methods as commonly used standards across multiple specialties, enhancing diagnostic accuracy while prioritizing patient safety.
Medical Applications and Procedures
Anatomical access points determine endoscopic selection, with flexible endoscopes and rigid endoscopes serving distinct clinical roles. Physiological openings or surgical portals guide instrument choice based on target structures and procedural objectives.
Flexible Endoscope Applications
Flexible endoscopes navigate body natural pathways through non-invasive approaches. Common procedures include gastroscopy for esophageal evaluation and bronchoscopy for airway inspection. These instruments traverse curved tract systems without external incisions, reducing recovery times.
Colonoscopic examinations demonstrate the diagnostic therapeutic capabilities of flexible systems. Integrated channels allow simultaneous tissue sampling and polyp removal. Such used procedures maintain mucosal integrity while providing real-time visualization of gastrointestinal surfaces.
Rigid Endoscope Applications
Rigid endoscopes require controlled surgical access points for sterile anatomical exploration. Orthopedic arthroscopy utilizes these devices for joint space visualization and cartilage repair. Their fixed structure enhances stability during intricate manipulations.
Abdominal laparoscopy exemplifies rigid endoscopic procedures in general surgery. Surgeons achieve precise organ examination through millimeter-scale ports. This approach minimizes tissue disruption compared to traditional open surgery, accelerating postoperative recovery.
Dual-scope adaptability occurs in urological and gynecological evaluations. Cystoscopy and hysteroscopy employ both modalities, selecting instruments based on anatomical complexity and clinical requirements.
How to describe the difference between rigid endoscopy and flexible endoscopy
Structural rigidity fundamentally determines endoscopic functionality across clinical scenarios. Material composition and operational mechanics create distinct advantages for each system, influencing their application in anatomical exploration.

Structural and Functional Variations
Flexible endoscopes employ pliable insertion tubes containing fiber-optic bundles and articulation mechanisms. These bendable components enable 180-degree angular adjustments at the distal tip, permitting navigation through curved body cavities like the colon or bronchi. Six structural elements – including a bending section and manipulation controls – work synergistically to maintain visualization during complex maneuvers.
Rigid endoscopes feature solid tubular construction with fixed optical pathways. Their non-articulating design limits insertion depth but provides superior stability during orthopedic or abdominal procedures. Five core components ensure optimal light transmission and image clarity in linear anatomical regions.
Differences in Procedural Control
Operational control mechanisms vary significantly between systems. Flexible instruments require precise manipulation of angulation dials to advance through tortuous pathways, demanding specialized technical expertise. Their flexible tube design permits deeper penetration into hollow organs compared to rigid counterparts.
Rigid systems maintain fixed positioning once inserted, allowing surgeons to execute procedures with millimeter-scale precision. This stability proves critical when operating in confined spaces like joint cavities, where unintended movement could compromise outcomes.
Advantages, Disadvantages, and Patient Outcomes
Clinical decision-making balances technical capabilities with patient-centered considerations when selecting endoscopic systems. Procedural success now extends beyond diagnostic accuracy to include recovery metrics and comfort levels.
Patient Comfort and Recovery
Flexible endoscopic approaches demonstrate superior tolerance profiles. Natural orifice access minimizes tissue disruption, reducing post-procedural pain. Most patients resume normal activities within hours compared to days-long recovery with rigid alternatives.
Real-time navigation through curved anatomy allows reach areas examination without surgical incisions. This decreases infection risks while maintaining mucosal integrity. However, slight image distortion may occur during complex maneuvers.
Comparative Imaging and Visualization Quality
Rigid systems provide unmatched visual clarity through direct optical pathways. High-definition imaging captures microscopic tissue details critical for orthopedic assessments. Stable platforms enable millimeter-scale precision during therapeutic interventions.
Despite requiring controlled surgical portals, this approach remains commonly used for abdominal evaluations. Patients undergoing rigid procedures often experience longer hospitalization stays due to anesthesia requirements and wound management needs.
- Flexible scopes reduce scarring risks through non-invasive access
- Rigid optics deliver superior resolution for critical diagnostics
- Recovery timelines vary significantly between modalities
Technological Innovations and Equipment Differences
Modern endoscopic systems demonstrate significant engineering evolution through integrated technology that enhances diagnostic and therapeutic precision. Component configurations vary across endoscope types, directly influencing their clinical performance and procedural adaptability.
Advancements in Imaging Systems
Contemporary endoscopes feature multi-lens arrays and advanced light transmission systems. High-definition cameras coupled with digital processors deliver 4K resolution imaging. These medical devices maintain visual clarity even in narrow anatomical spaces.
The distal tip of flexible tube systems integrates multiple functional ports. A shared air-water nozzle expands cavities while cleansing the lens during examinations. Integrated biopsy forceps channels enable simultaneous tissue sampling and fluid management.
Rigid endoscope products exhibit streamlined designs for specialized applications. Many lack auxiliary channels in procedures requiring minimal intervention, such as arthroscopy. This configuration prioritizes optical performance over multifunctionality.
Manufacturers continue refining diagnostic therapeutic capabilities through micro-optics and enhanced light guides. These innovations reduce instrument diameters while improving image fidelity across diverse systems. Such progress supports targeted interventions with reduced patient trauma.
Conclusion
Clinical success with endoscopic procedures hinges on matching instrument capabilities to anatomical demands. Rigid endoscopes remain preferred for linear pathways requiring stable visualization, while flexible systems excel in navigating curved body structures. This fundamental distinction guides equipment selection across specialties.
Technological advancements enhance both types of endoscopes, improving precision in diagnostic and therapeutic applications. Modern flexible tube designs now incorporate advanced lens configurations and biopsy forceps integration without compromising maneuverability. Simultaneously, rigid products maintain superiority in high-resolution imaging for joint and abdominal evaluations.
Practitioners must weigh multiple factors when choosing systems: target anatomy depth, required control levels, and patient recovery expectations. These decisions directly influence procedural efficacy and clinical outcomes. As technology evolves, hybrid approaches may further bridge current functional differences between endoscopic platforms.
FAQ
How do rigid and flexible endoscopes differ structurally?
Rigid endoscopes utilize straight stainless-steel tubes with fixed lenses, optimized for high-resolution imaging in accessible anatomical regions. Flexible endoscopes employ bendable fiber-optic or digital insertion tubes, enabling navigation through curved pathways like the gastrointestinal tract. Brands such as Olympus and Karl Storz engineer distinct optical systems for each type.
Which procedures typically require flexible endoscopy?
Flexible endoscopy is standard for colonoscopies, upper GI evaluations, and bronchoscopies due to its ability to traverse body cavities with complex geometries. Devices like Medtronic’s colonoscopes integrate biopsy forceps and irrigation channels for therapeutic interventions in the lower digestive tract.
Why are rigid endoscopes preferred in arthroscopy and laparoscopy?
The unyielding construction of rigid endoscopes from manufacturers like Stryker ensures stability during precise joint or abdominal cavity examinations. Their superior light transmission and 4K imaging support real-time surgical instrument manipulation in orthopedic and gynecological operations.
How does patient experience vary between the two endoscopic methods?
Flexible endoscopic procedures often require sedation for comfort during insertion through tortuous anatomy, while rigid endoscopy under general anesthesia minimizes movement in sterile operative fields. Recovery timelines differ based on procedural invasiveness and anesthesia type.
What technological advancements differentiate modern endoscope systems?
Innovations like Boston Scientific’s laser-confocal endoscopy enhance cellular-level visualization in flexible models. Rigid systems incorporate rod-lens technology from Wolf Medical for distortion-free imaging during minimally invasive neurosurgery or urologic interventions.
Are there limitations to using flexible endoscopes in diagnostic applications?
While adaptable, flexible endoscopes may compromise image clarity compared to rigid counterparts in narrow luminal spaces. Certain therapeutic maneuvers—like polyp resection in angled colonic segments—require specialized training to maintain procedural accuracy.
How do sterilization protocols differ between endoscope types?
Autoclavable rigid endoscopes from Aesculap allow steam sterilization, whereas flexible models from Pentax demand meticulous high-level disinfection due to heat-sensitive components. Reprocessing standards follow FDA guidelines to prevent cross-contamination risks.