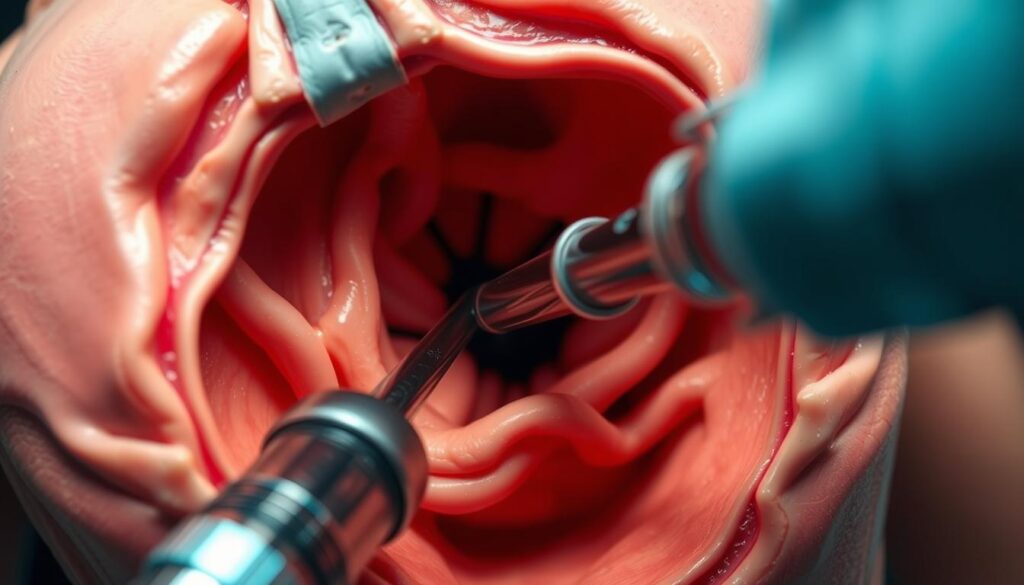
Endoscope torque control emerges as a cornerstone in contemporary medical practices, delivering unmatched precision in both diagnostic and therapeutic endeavors. This skill empowers healthcare professionals to adeptly traverse the intricacies of anatomical structures. Achieving mastery in precise endoscope steering is imperative for ensuring superior patient outcomes and the overall success of procedures1.
Research elucidates the subtle force dynamics inherent in endoscopic procedures. The mean push/pull force recorded is 3.64 N, accompanied by a mean torque of 3.3 N-mm, illustrating the delicate equilibrium required for effective manipulation1. These metrics underscore the critical role of refined control methodologies in the realm of minimally invasive surgeries.
The importance of endoscope torque control is further accentuated by its extensive application. In South Korea, where gastric cancer incidence is significantly high, esophagogastroduodenoscopy (EGD) has emerged as a ubiquitous medical procedure2. This widespread adoption highlights the imperative for proficiency in endoscopic techniques to guarantee accurate diagnoses and treatments.
Attaining proficiency in endoscope steering entails a formidable learning journey. Practitioners must hone a range of skills, from rudimentary tip deflection to sophisticated paradoxical movement techniques2. This complexity demands rigorous training programs and the integration of innovative technologies to elevate procedural accuracy and safeguard patient well-being.
Key Takeaways
- Endoscope torque control is critical for precise medical procedures
- Mean push/pull force and torque measurements guide optimal control
- EGD is a widely used diagnostic tool, significantly in high-risk areas
- Mastering endoscope steering necessitates extensive training and practice
- Advanced technologies are improving precision in endoscopic procedures
Understanding Endoscope Force Dynamics
In the realm of minimally invasive surgery (MIS), the dynamics of endoscope force are of utmost significance. These procedures necessitate incisions ranging from 0.5 to 1.5 cm, underscoring the imperative for precise force application3.
Basic Principles of Force Application
The art of force application in endoscopy revolves around a nuanced interplay of push/pull forces and rotational torques. The endoscope’s maneuverability hinges on the synergy between these forces and the gastrointestinal tract’s frictional resistance. For effective control, the frictional force must be robust enough to counteract horizontal magnetic forces4.
Force and Torque Interaction Patterns
The relationship between force and torque in endoscopic interventions is intricately complex. For capsule endoscopes, the vertical magnetic force must surpass the device’s weight for accurate positioning. The static friction force must be at least equal to or greater than the horizontal magnetic force to arrest translational motion4. These interactions are vital for the endoscope’s navigation through the body’s convolutions and bends.
Impact of User Experience on Force Control
User experience profoundly influences force control in endoscopic procedures. Novice practitioners often face challenges with depth perception and horizon stability when employing flexible endoscopes. Skilled operators, through experience, develop a refined sense of the required force application, significantly boosting their capacity for precise incisions3. This expertise is critical, given the limitations of current endoscopes, such as the absence of stiffness control in flexible types or the diminished working space of rigid endoscopes.
Grasping these endoscope force dynamics and force application principles is fundamental to the advancement of minimally invasive surgery and the enhancement of patient outcomes.
The Science Behind Endoscope Torque Control
In the realm of modern medical procedures, the science of endoscope torque control is of utmost importance. The intricacy of these instruments necessitates the implementation of advanced torque control mechanisms. These are essential for ensuring precise navigation within the human body. At the core of many endoscopes lies the Tendon-Sheath-Mechanism (TSM), a system that facilitates flexible movement.
The colon, a primary focus for endoscopic interventions, presents unique challenges. Its length, approximately 180 cm, and varying diameters, ranging from 34.5 mm to 75 mm, demand meticulous maneuvering. The presence of at least three major anatomic turns, with bends exceeding 90 degrees, further complicates navigation5.
Endoscope torque control mechanisms must account for these anatomical complexities. Traditional endoscopes often induce significant tissue stress, leading to patient discomfort and the need for sedation. This has prompted the development of tethered magnetic capsules, aiming to reduce tissue stress and enhance patient comfort5.
Advanced torque control systems in robotic-assisted surgeries have shown significant improvements. They can diminish hand tremor by up to 87% and enhance motion scaling by 3-5 times, significantly increasing precision6. Despite these advancements, challenges persist. High pre-tension in tendons can result in interaction forces exceeding 20 Newtons, potentially damaging surrounding tissues6.
The science of endoscope torque control continues to evolve. Researchers are exploring compliant mechanisms to reduce stiffness, as traditional actuators can be up to 90% stiffer than their compliant counterparts. This focus on flexibility and precision aims to revolutionize endoscopic procedures, making them safer and more effective for patients.
Essential Components of Endoscopic Force Measurement
Endoscopic force measurement is indispensable for the precise control required in medical procedures. This discourse delves into the fundamental components that facilitate accurate force detection and measurement within endoscopic instruments.
Load Cell Integration Systems
Load cells are the cornerstone of force measurement in endoscopes. These systems employ strain gauges to detect applied forces. Contemporary load cells are capable of withstanding standard sterilization protocols, including steam at 121 °C and 205 kPa for 4 to 15 minutes7. Certain advanced load cells, such as those utilizing FUSED isolator technology, can endure hundreds to thousands of autoclave cycles, ensuring enduring reliability7.
Force Sensor Technologies
Force sensor technologies have advanced to meet the rigorous demands of endoscopic applications. The QLA414 Nano Force Sensor, measuring just 4 mm x 5 mm, represents this advancement7. It offers high accuracy in 5 lb and 10 lb capacities, with a natural frequency response up to 98 kHz7. Some sensors, as small as 3 mm x 4 mm, can measure forces up to 50 lb7.
Measurement Accuracy Parameters
Accuracy is of utmost importance in endoscopic force measurement. The QLA414 Nano Force Sensor boasts a nonlinearity specification of ±0.5% of rated output in its 5 lb and 10 lb capacities7. It features a safe overload capacity of up to 200% and can measure ultra-low deflections of 0.0002 inches (0.005 mm)7. These parameters ensure precise force detection during delicate procedures.
| Parameter | Value |
|---|---|
| Sensor Size | 4 mm x 5 mm |
| Force Capacity | 5 lb and 10 lb |
| Frequency Response | Up to 98 kHz |
| Nonlinearity | ±0.5% of rated output |
| Safe Overload | Up to 200% |
The Colonoscopy Force Monitor (CFM) exemplifies cutting-edge force measurement technology in endoscopy. It records forces and torques at 7.5 measurements per second, allowing for the calculation of over 20 force-related parameters8. This level of detail enables the identification of differences in endoscopic techniques among experienced practitioners8.
Challenges in Maintaining Precise Control
Endoscope control challenges pose formidable obstacles in medical procedures. Physicians encounter a spectrum of musculoskeletal injuries during ERCP procedures, underscoring the physical demands of endoscope manipulation9. The precision required in endoscopic interventions is critical, yet numerous factors complicate this objective.
Common Control Issues
The Tendon-Sheath-Mechanism (TSM) employed in endoscopic driving exhibits a “dead zone” during motion, affecting control accuracy9. This phenomenon, coupled with compliance and friction in snake bone structures, imposes precise control limitations9. Surgeons frequently rely on visual feedback alone due to the absence of haptic sensation in robotic instruments6.
Environmental Factors
Environmental conditions significantly influence endoscopic procedures. The force required during transgastric appendectomy is 8 N, whereas transperineal appendectomy necessitates 16 N1. These variations necessitate adaptive control strategies. During colonoscopy, peak pushing and pulling forces reach 43 N and 17 N respectively, with clockwise and counter-clockwise torques of 0.8 Nm and 1 Nm1.
Technical Limitations
Endoscope designs confront technical constraints. Modified endoscopes with 16 mm diameters, compared to standard 12 mm ones, may induce increased patient discomfort9. High tendon pre-tension in robotic endoscopes can lead to stiff actuation, risking tissue damage in 14% of high-force cases6. The learning curve for minimally invasive surgeries is steep, with 60-70% of surgeons feeling they need more training to achieve proficiency6.
| Procedure | Force Range (N) | Torque Range (N-mm) |
|---|---|---|
| Traditional Laparoscopic Surgery | 0-10 | 0-100 |
| Appendectomy (Mean Push/Pull) | 3.64 (σ = 3.54) | 3.3 (σ = 38.6) Counter-clockwise |
These technical limitations highlight the complexity of achieving precise control in endoscopic procedures, necessitating ongoing research and development in the field1.
Advanced Technologies in Torque Measurement
Endoscope torque sensors have undergone a transformative evolution, introducing unparalleled precision to the realm of medical procedures. The advent of miniaturized strain gauge-based sensors and fiber Bragg grating (FBG) systems marks a significant milestone. These innovations facilitate real-time feedback, significantly improving control during endoscopic interventions.
Strain gauge torque sensors leverage electric measurement technology to achieve accurate torque detection10. In contrast, non-contact torque sensors, which employ torsion bar mechanisms, offer unparalleled precision without necessitating physical connections. Their applications span diverse sectors, from automotive engines to automatic machine tools10.
The FUTEK NanoSensor QLA414, measuring a mere 4mm x 5mm, epitomizes a paradigm shift in compact force measurement. It supports capacities of 5 lb and 10 lb, coupled with an ultra-low deflection of 0.0002″ (0.005 mm)11. Its diminutive size and exceptional performance render it an exemplary choice for integration into endoscopic instruments.
Calibration is indispensable for ensuring the accuracy of torque measurements. The calibration process aims for an error range of 0.01gf.cm to 0.03gf, with annual recalibration cycles being the norm10. Equally critical is the proper installation, necessitating a concentricity of sensor and equipment axes within φ 0.05mm to guarantee precise measurements10.
These cutting-edge torque measurement technologies are revolutionizing endoscopic procedures, delivering enhanced precision and control. As advancements continue, we anticipate further miniaturization and enhanced sensor capabilities, paving the way for even more refined endoscopic methodologies.
Ergonomic Considerations for Operators
In the realm of modern medical procedures, endoscope ergonomics emerge as a critical factor. Given that 61% of gastroenterologists spend over 40% of their time on endoscopic tasks, prioritizing operator comfort is imperative12. The alarming rate of endoscopy-related injuries (ERIs), ranging from 39% to 89% among gastroenterologists, further emphasizes this necessity12.
Optimal Handling Techniques
Adopting proper handling techniques is fundamental to mitigating physical strain during endoscopic procedures. A Rapid Entire Body Assessment revealed that 32% of endoscopy procedures involve postures potentially leading to musculoskeletal discomfort13. To counteract this risk, endoscopists must strive to maintain neutral postures and utilize instruments designed with ergonomics in mind.
Reducing Operator Fatigue
Operator fatigue reduction is a critical concern within endoscopic practice. It is noteworthy that 75% of gastroenterologists employ devices lacking adequate ergonomic features13. The integration of ergonomic tools can enhance procedural efficiency by up to 50% and shorten surgery duration by 20%13. Implementing microbreaks and scheduled macrobreaks during procedures can also significantly reduce the risk of ERIs12.
Safety Protocols
Implementing robust safety protocols is essential for preventing ERIs. Ergonomic training programs have shown a 40% effectiveness rate in injury reduction13. Recommendations include maintaining a neutral monitor position during endoscopies and conducting regular ergonomic assessments. These measures have resulted in a 30% decrease in injury claims among staff1213.
| ERI Location | Prevalence | Confidence Interval |
|---|---|---|
| Hands and fingers | 35.8% | 18.1-58.6% |
| Back | 35.3% | 24.3-48% |
| Upper back and neck | 32.6% | 21.3-46.3% |
| Thumb | 29.2% | 16.3-46.7% |
| Neck | 26.1% | 16.9-37.9% |
Role of Haptic Feedback Systems
Haptic feedback systems are indispensable in the realm of endoscope torque control and surgical precision enhancement. They furnish operators with tactile information, significantly augmenting the accuracy and safety of endoscopic interventions.
Types of Haptic Technologies
Force feedback and tactile displays constitute the primary categories of haptic technologies employed in medical contexts. Force feedback systems replicate the forces applied during procedures, whereas tactile displays simulate textures and surface properties. In robotic colonoscopy, haptic feedback has proven to be highly beneficial. The maximum insertion force recorded was approximately 10 N, with an average of 4 N. The maximum torque in rotation was roughly 0.2 Nm14.
Implementation Strategies
Integrating haptic feedback into endoscopic systems necessitates overcoming challenges such as size constraints and sterilization requirements. Incisions for minimally invasive surgery span from 5 mm to 15 mm, posing a significant limitation on sensor integration15. The need for robust sensor designs is underscored by the necessity for autoclave sterilization, which operates at 121 °C and 205 kPa steam for 4 to 15 minutes15.
Benefits for Surgical Precision
Endoscope haptic feedback substantially enhances surgical precision. A comparative study between colonoscopies with and without haptic feedback revealed notable improvements. Procedures with feedback exhibited reduced insertion times (70 seconds vs 87 seconds) and lower maximum pull forces (5.27 N vs 7.34 N)16. Haptic feedback also significantly diminished the incidence of sigmoid colon overstretching, from 32% to 8%, underscoring its capacity to enhance patient safety and procedure outcomes16.
Advancements in haptic technology are revolutionizing endoscopic procedures, enabling more precise and safer interventions. This represents a significant advancement in surgical precision enhancement.
Training Requirements for Precise Control
Endoscope control training is imperative for the acquisition of medical procedure skills. A study, involving 29 participants, including 13 seasoned colonoscopists and 16 novices, underscored the significance of structured training programs17. The research demonstrated that novices significantly enhanced their completion time and consistency in endoscope tip control following a six-session training program17.
Precision skill development in endoscopy necessitates mastery of core technical, nontechnical, and cognitive skills18. These encompass correct positioning of the endoscope, effective advancement techniques, and loop reduction18. Trainees must also acquire the ability to evaluate patient suitability and risks, highlighting the critical role of extensive medical knowledge18.
The Joint Advisory Group on GI Endoscopy (JAG) establishes stringent standards for endoscopists. For provisional certification, endoscopists must conduct procedures independently, with a supervisor available for complex cases19. Full certification requires over 200 lifetime endoscopic procedures, with serious complication rates below 0.5%19.
Effective training paradigms frequently incorporate simulation-based training and haptic-enabled systems. These methodologies have been shown to be invaluable in augmenting operator skills and patient safety. By prioritizing structured learning and continuous assessment, medical institutions can guarantee that endoscopists attain the precise control essential for successful procedures.
Future Developments in Endoscopic Control
The realm of endoscopy is poised on the cusp of a technological upheaval. Upcoming endoscope control systems are destined to redefine the landscape of medical procedures, promising heightened precision and operational efficiency.
Emerging Technologies
Wireless capsule endoscopy (WCE) has emerged as a focal point in medical robotics research. The evolution of these devices, initially 11 x 26 mm in size, has been substantial, with the first commercially available capsule receiving medical certification in 200120. These advancements are powered by silver oxide button batteries, enabling 8-10 hours of operation at a power consumption of approximately 20 mW20.
Artificial Intelligence Integration
The integration of AI in endoscopy is poised to transform diagnostic processes. Future intelligent capsule endoscopy robots are anticipated to possess enhanced endurance, active motion navigation, and high-speed bi-directional communication capabilities20. AI-driven algorithms for lesion classification are in development, aiming to expedite inspections by automatically detecting anomalies20.
Robotic Assistance Systems
The notion of the “capsule surgeon” is gaining momentum, potentially enabling autonomous minimally invasive surgeries without direct physician oversight20. Innovations such as near-field wireless power transmission and magnetic field active drive are being explored for WCE enhancements20. These advancements are expected to elevate the efficacy of endoscopic procedures, leading to improved patient outcomes and broadening the scope of minimally invasive diagnostics and treatments.
Quality Assurance and Maintenance
In the realm of medical diagnostics, the maintenance and quality assurance of endoscopes are indispensable. These procedures are critical for ensuring the precision and safety of diagnostic and therapeutic interventions. The meticulous upkeep of endoscopes guarantees the accurate application of torque, a factor that significantly impacts patient outcomes.
Calibration Procedures
The calibration of endoscopes is fundamental to their accuracy. It necessitates adherence to rigorous protocols, which involve the calibration of force sensors and torque measurement systems. This calibration process is validated against established benchmarks, ensuring the reliability of the data obtained during procedures.
Regular Maintenance Protocols
Endoscope maintenance encompasses a range of activities, including thorough cleaning, sterilization, and inspection. These protocols are designed to prevent the transmission of infections. The efficacy of these measures is underscored by the low infection rate during gastrointestinal endoscopy, estimated at 1 in 10 million procedures when adherence to protocols is strict21.
- Clean all channels and surfaces
- Sterilize using approved methods
- Inspect for wear and damage
- Replace parts as needed
Performance Monitoring
Continuous monitoring is imperative for ensuring the quality of endoscopes. Technicians must track and analyze various performance indicators to detect any anomalies. This proactive monitoring is essential for maintaining the high standards required in endoscopic procedures.
| Metric | Target | Frequency |
|---|---|---|
| Bacterial load | <10^2 CFU/mL | After each use |
| Torque accuracy | ±5% of calibrated value | Monthly |
| Image quality | Clear, no artifacts | Weekly |
Manual cleaning can significantly reduce microbial loads, achieving a 99.99% reduction in microorganisms21. The regular implementation of maintenance and quality control measures is vital for ensuring the safety and efficacy of endoscopes in clinical settings.
Conclusion
The domain of endoscope torque control advancements has witnessed an extraordinary evolution, profoundly influencing the trajectory of endoscopic precision. Recent investigations underscore the substantial enhancements in performance metrics, evident when robotic modes are employed as opposed to manual operation22.
Advancements in technology have significantly expanded the capabilities of endoscopic systems. Contemporary systems now accommodate a variety of rigid laparoscopes and facilitate integration with six degree-of-freedom robotic manipulators, providing enhanced control and adaptability22. These innovations have resulted in superior torque control, with certain systems limiting tip torque to 1.0Nm and setting angular velocities at 50 rpm for optimal performance23.
The repercussions of these advancements on surgical practices are profound. In simulated transgastric appendectomy, mean push/pull forces of 3.64 N have been documented, alongside torque measurements that reflect precise control capabilities1. These statistics highlight the escalating precision in endoscopic interventions, heralding a future of less invasive and more precise surgical endeavors.
As we anticipate the future of endoscopic precision, ongoing research and development in force measurement, ergonomic design, and robotic assistance systems hold promise for further refinement of surgical outcomes and patient care. The ongoing progression of endoscope torque control advancements will undoubtedly be instrumental in shaping the future of minimally invasive medical procedures.
FAQ
What is endoscope torque control?
Why is understanding force dynamics important in endoscopy?
What are the main challenges in maintaining precise endoscope control?
How do advanced torque measurement technologies improve endoscopic procedures?
What ergonomic considerations are important for endoscope operators?
How does haptic feedback enhance endoscope torque control?
What training is required to achieve precise endoscope control?
How might artificial intelligence impact future endoscope control?
What are the key aspects of quality assurance for endoscopic systems?
How do load cells contribute to endoscopic force measurement?
Source Links
- Characterization of Force and Torque Interactions during a Simulated Transgastric Appendectomy Procedure – https://pmc.ncbi.nlm.nih.gov/articles/PMC4344408/
- Technical skills and training of upper gastrointestinal endoscopy for new beginners – https://pmc.ncbi.nlm.nih.gov/articles/PMC4299329/
- A review on recent advances in soft surgical robots for endoscopic applications – https://pmc.ncbi.nlm.nih.gov/articles/PMC6771908/
- Optimal Motion Control of a Capsule Endoscope in the Stomach Utilizing a Magnetic Navigation System with Dual Permanent Magnets – https://www.mdpi.com/2072-666X/15/8/1032
- Closed Loop Control of a Tethered Magnetic Capsule Endoscope – https://www.roboticsproceedings.org/rss12/p18.pdf
- Control Evaluation of Antagonistic Series Elastic Actuation for a Robotic Endoscope Joint – Journal of Bionic Engineering – https://link.springer.com/article/10.1007/s42235-022-00180-6
- FUTEK Advanced Sensor Technology – https://www.futek.com/applications/Endoscope-Force-Control?srsltid=AfmBOoqatilcmPEP54Luf9j6hUU6CyeZK0Y2Fudl5bIUN3vc6eForXal
- Characterization of forces applied by endoscopists during colonoscopy by using a wireless colonoscopy force monitor – https://pmc.ncbi.nlm.nih.gov/articles/PMC2822026/
- Safety-Centric Precision Control of a Modified Duodenoscope Designed for Surgical Robotics – https://www.mdpi.com/2075-1702/12/8/500
- Torque Sensor & Transducer | ATO.com – https://www.ato.com/torque-sensor?srsltid=AfmBOoorUx2vkbbh-U-W7f83x7e_fKgBKt_pkrHC5wTR5_cksFApiYp0
- FUTEK Advanced Sensor Technology – https://www.futek.com/applications/Endoscope-Force-Control?srsltid=AfmBOoppjnvcQIAoUxLraygZ2ijv3Q2GMSzqWH7XZBafMWolz_mTCJpn
- American Society for Gastrointestinal Endoscopy guideline on the role of ergonomics for prevention of endoscopy-related injury: summary and recommendations – https://www.asge.org/docs/default-source/guidelines/asge-guideline-on-the-role-of-ergonomics-summary.pdf
- ASGE Guideline on the Role of Ergonomics for Prevention of Endoscopy-related Injury (ERI): Summary and Recommendations – https://scholarworks.indianapolis.iu.edu/bitstreams/a89d0d0c-7cef-4a22-88bc-722545b0d390/download
- Development of a Robotic Colonoscopic Manipulation System, Using Haptic Feedback Algorithm – https://pmc.ncbi.nlm.nih.gov/articles/PMC5122629/
- FUTEK Advanced Sensor Technology – https://www.futek.com/haptic-feedback-robotic-surgery?srsltid=AfmBOorHvP0seRaxatn03rDH7amHQpYAVemoU51f-JX_QsGwPI1F8LMq
- Haptic feedback is useful in remote manipulation of flexible endoscopes – https://pmc.ncbi.nlm.nih.gov/articles/PMC6133662/
- A novel training device for tip control in colonoscopy: preliminary validation and efficacy as a training tool – https://pmc.ncbi.nlm.nih.gov/articles/PMC5715030/
- Colonoscopy core curriculum – https://www.asge.org/docs/default-source/default-document-library/colonoscopy-core-curriculum.pdf
- Gastroenterology Education and CPD for trainees and specialists » JAG Portfolio – https://www.gastrotraining.com/category/endoscopy/general/jag-requirement
- Robotic wireless capsule endoscopy: recent advances and upcoming technologies – Nature Communications – https://www.nature.com/articles/s41467-024-49019-0
- Endoscopy – https://www.cancertherapyadvisor.com/home/decision-support-in-medicine/hospital-infection-control/endoscopy/
- A generic scope actuation system for flexible endoscopes – Surgical Endoscopy – https://link.springer.com/article/10.1007/s00464-023-10616-7
- A novel gaze-controlled flexible robotized endoscope; preliminary trial and report – Surgical Endoscopy – https://link.springer.com/article/10.1007/s00464-021-08556-1