Modern endoscopic approaches have revolutionized the management of colorectal strictures, offering a minimally invasive alternative to surgical reoperation. These methods are particularly significant in treating benign anastomotic strictures, where early intervention can prevent complications and improve patient outcomes1.
Endoscopic balloon dilation is one of the most commonly used techniques, with success rates reported in approximately 20% of patients1. However, in cases where this method fails, alternatives like the Magnetic Compression Technique (MCT) have shown promise. MCT involves placing magnets on either side of the stenosis to create an anastomosis, which can be particularly effective in patients with heavy scar tissue1.
Proper bowel preparation is crucial to reduce the risk of perforation, which is higher with hydrostatic balloon dilation (4.6%)2. Mechanical perforation can occur at sites of weakness, such as strictures, making careful technique selection essential2. The choice of procedure should be based on stricture etiology and location to ensure optimal results.
Key Takeaways
- Modern endoscopic methods provide a less invasive option for managing colorectal strictures.
- Early intervention in benign anastomotic strictures can prevent complications.
- Endoscopic balloon dilation is effective in about 20% of cases.
- Magnetic Compression Technique (MCT) is a viable alternative when balloon dilation fails.
- Proper bowel preparation reduces the risk of perforation during procedures.
Understanding Colorectal Strictures
Colorectal strictures are a significant clinical challenge, often requiring tailored interventions based on their underlying causes. These narrowings in the colon or rectum can result from various factors, including surgery, inflammation, and radiation therapy. Identifying the root cause is crucial for effective management and improved patient outcomes.
What Causes Benign Colorectal Strictures?
Post-surgical fibrosis is a primary cause of benign colorectal strictures, particularly after procedures like low anterior resection. Studies show a 59% success rate in cancer cases compared to 88% in benign cases3. This highlights the importance of early intervention in non-malignant strictures.
Radiation-induced ischemia also plays a role, contributing to chronic inflammation and fibrosis3. Patients who undergo pre-operative radiation are at higher risk of developing severe strictures3. This underscores the need for careful patient evaluation before treatment.
Inflammatory bowel disease (IBD), particularly Crohn disease, is another common etiology. The pathophysiology of Crohn-related strictures differs from anastomotic strictures, requiring distinct therapeutic approaches4.
Endoscopic submucosal dissection (ESD) techniques can also lead to stricture formation, with complications like perforation increasing the risk5. Advanced closure methods, such as endoclips, may mitigate this risk but require further study.
| Cause | Incidence | Key Factors |
|---|---|---|
| Post-surgical fibrosis | 5-20% after low anterior resection3 | Higher success in benign cases |
| Radiation-induced ischemia | Correlates with pre-operative radiation3 | Chronic inflammation pathways |
| Crohn disease | Common in IBD patients4 | Distinct pathophysiology |
| Endoscopic submucosal dissection | 75% lumen occupation3 | Risk of perforation |
Understanding these causes helps clinicians choose the most effective treatment strategies. Whether addressing benign colorectal anastomotic strictures or those related to Crohn disease, a tailored approach ensures better outcomes.
Colonoscopy Technique for Stricture Dilation: An Overview
Endoscopic methods have become a cornerstone in addressing narrowing of the colorectal lumen, offering precise and effective solutions. With an 86% immediate success rate for balloon dilation, these techniques are highly reliable for symptom relief6. Long-term efficacy stands at 58%, making them a sustainable option for many patients6.
Mechanical and pneumatic dilation systems are often compared for their effectiveness. Mechanical systems provide controlled force, while pneumatic systems offer flexibility in complex cases7. Fluoroscopic guidance plays a critical role in navigating intricate strictures, ensuring accurate placement and reducing complications7.
Technical considerations vary based on stricture location. Rectal strictures may require additional techniques like endoscopic stricturotomy, while colonic strictures often respond well to standard dilation methods6. For complete lumen obstruction, stents and rendezvous techniques are employed to restore patency7.
The evolution from surgical to endoscopic first-line approaches has significantly improved patient outcomes. This shift is supported by advanced tools and techniques, making endoscopic management the preferred choice for many clinicians7.
Endoscopic Balloon Dilation: The First-Line Treatment
Endoscopic balloon dilation stands as a primary intervention for addressing narrowing in the colorectal lumen. This minimally invasive procedure is favored for its precision and ability to provide immediate symptom relief. It is particularly effective in treating benign strictures, offering a reliable alternative to surgical reoperation.
How Balloon Dilation Works
The procedure involves the use of CRE™ multidiameter balloons, which apply radial force to expand the narrowed lumen. A sequential dilation protocol is typically followed, starting with a 12mm balloon and progressing to 15mm. This gradual approach minimizes tissue trauma and reduces the risk of complications.
Standard inflation pressure is maintained at 3 atm, ensuring controlled and safe dilation. Fluoroscopic guidance is often employed to enhance accuracy, particularly in complex cases. This method allows clinicians to navigate intricate strictures with precision.
Success Rates and Predictors
Studies report an immediate symptom relief rate of 77%, with long-term success observed in 44% of patients3. For Crohn’s-related strictures, the success rate is slightly higher at 62%3. These outcomes highlight the effectiveness of balloon dilation treatment in diverse clinical scenarios.
Predictive factors for success include stricture length under 4cm and diameter less than 10mm. Patients meeting these criteria are more likely to achieve favorable outcomes. However, recurrence rates remain a concern, with 25% of patients experiencing restenosis within five years3.
Complication rates are relatively low, with perforation occurring in 1.85% of cases3. This underscores the importance of careful patient selection and procedural technique. By adhering to established protocols, clinicians can optimize the success rate and minimize risks.
Preparing for the Procedure
Proper preparation is essential to ensure the safety and success of procedures addressing colorectal narrowing. This involves thorough patient evaluation, risk assessment, and adherence to specific bowel preparation protocols. These steps minimize complications and optimize outcomes.
Patient Evaluation and Risk Assessment
Before any intervention, a detailed patient evaluation is critical. This includes reviewing medical history, particularly prior abdominal surgeries or radiation therapy, which can influence procedural risks2. Imaging studies, such as CT scans, are mandatory to exclude malignant strictures and characterize the narrowing8.
Risk stratification is particularly important for immunocompromised patients. Factors like age, with a mean of 64.6±10.7 years in a 40-case study, must also be considered8. Anesthesia considerations are tailored for patients with radiation-damaged tissue to ensure safety during the procedure.
Bowel Preparation Protocols
Effective bowel preparation is a cornerstone of procedural success. Protocols using MiraLAX and polyethylene glycol (PEG) solutions are commonly employed to ensure a clear field of view8. Enhanced protocols are recommended for patients with post-surgical anatomy to address unique challenges.
Antibiotic prophylaxis is another critical component. Guidelines recommend regimens such as ampicillin, amoxicillin, gentamicin, and vancomycin for high-risk patients8. This reduces the risk of infection and supports optimal recovery.
Carbon dioxide insufflation is often used during the procedure to minimize distention and reduce the risk of ischemia2. These measures, combined with thorough preparation, ensure a safer and more effective intervention.
Step-by-Step Guide to Balloon Dilation
Balloon dilation is a precise method for managing narrowing in the colorectal lumen, offering immediate relief and long-term benefits. This procedure is particularly effective for anastomotic strictures, where careful technique ensures optimal outcomes. The process involves positioning, balloon selection, inflation, and post-dilation assessment, each critical to success.
Positioning and Scope Insertion
Proper patient positioning is essential for effective dilation. The left lateral decubitus position is commonly used, allowing optimal access to the colorectal lumen9. A flexible sigmoidoscope is inserted to visualize the narrowing, ensuring accurate placement of the balloon catheter.
In cases of complete obstruction, guidewire techniques are employed to navigate the stricture. This approach enhances precision and reduces the risk of complications7.
Balloon Selection and Inflation
Multidiameter balloons, typically 5.5cm in length, are selected based on stricture characteristics. Sequential dilation is performed, starting with smaller diameters and gradually increasing to minimize tissue trauma7.
Inflation protocols include a 5-minute dwell time per diameter increment. This ensures controlled expansion and reduces the risk of perforation9.
Post-Dilation Assessment
After dilation, imaging protocols such as abdominal X-rays are used to assess outcomes and detect complications like perforation9. Criteria for same-session repeat dilation include persistent symptoms or incomplete lumen expansion.
Post-procedure monitoring is critical to ensure patient safety and evaluate the effectiveness of the intervention.
| Step | Key Details | Duration |
|---|---|---|
| Positioning | Left lateral decubitus position | 5-10 minutes |
| Balloon Selection | 5.5cm multidiameter balloon | 10-15 minutes |
| Inflation | 5-minute dwell time per increment | 15-20 minutes |
| Post-Dilation | Abdominal X-ray for assessment | 5-10 minutes |
This structured approach ensures the safe and effective use of balloon dilation for managing colorectal narrowing. By adhering to these steps, clinicians can achieve favorable outcomes and minimize risks.
Self-Expandable Metal Stents (SEMS) for Refractory Cases
Self-expandable metal stents (SEMS) offer a reliable solution for refractory cases of colorectal narrowing. These devices are particularly effective when traditional methods fail, providing a minimally invasive option for complex strictures. With a clinical success rate of 81% despite migration, SEMS have become a cornerstone in endoscopic management of challenging cases10.

Types of SEMS: Covered vs. Uncovered
SEMS are available in two primary types: covered and uncovered. Covered stents, such as Hanarostent, are designed to prevent tissue ingrowth but have a higher migration rate of 63%10. Uncovered stents, like Wallflex, allow for epithelialization, with rates of 17% observed at 16.7 months3. The choice between these types depends on stricture characteristics and treatment goals.
Placement Techniques and Challenges
Placement of SEMS requires precision and expertise. Techniques like through-the-scope (TTS) clips and endoscopic suturing are used to anchor stents, reducing migration risks3. In a study, TTS clips showed a 0% migration rate in a 7-patient case series3. However, challenges remain, particularly in proximal colonic stents, where migration management protocols are critical.
Despite these challenges, SEMS have shown significant success in treating refractory benign strictures. The FDA currently approves SEMS for palliative use but not for colorectal anastomotic strictures in the U.S3.. This highlights the need for continued research and innovation in stents treatment benign cases.
Biodegradable Stents: A Promising Alternative
The development of biodegradable stents offers a promising alternative for patients with treatment refractory cases. These stents, composed of polydioxanone polymers, provide a temporary solution for managing narrowing in the colorectal lumen. In an 11-patient study, they demonstrated a 45% success rate, making them a viable option for complex cases11.
Polydioxanone-based stents degrade completely within 11-12 weeks, eliminating the need for endoscopic removal11. This degradation timeline is particularly beneficial for patients with postsurgical strictures, where long-term stent placement may not be ideal. However, these stents are associated with a higher rate of adverse events (28.6%) compared to fully covered self-expanding metal stents (10.6%)12.
Material science plays a critical role in the effectiveness of biodegradable stents. Poly-L-lactic and polydioxanone polymers are commonly used, with polydioxanone providing radial force for 4-5 weeks before degradation12. This makes them suitable for managing stricture formation in postsurgical cases and fistula combinations.
Despite their advantages, biodegradable stents have limitations. Migration risk is higher in proximal colon applications, with rates of 28.6% observed in some studies12. Future directions include the development of antimigration designs and more flexible systems to improve efficacy in challenging environments10.
Comparative cost analysis shows that biodegradable stents may offer better long-term outcomes than permanent SEMS but with higher adverse event rates12. This highlights the need for careful patient selection and continued innovation in stent technology to address treatment refractory cases effectively.
Combined Techniques for Complex Strictures
Advanced hybrid methods are reshaping the treatment of complex colorectal conditions. These combined techniques integrate multiple tools and approaches to address challenging cases effectively. By leveraging the strengths of different methods, clinicians can achieve better outcomes for patients with refractory strictures.
Electroincision with Balloon Dilation
The combination of electrocautery and balloon dilation has shown remarkable success in managing strictures following surgery or inflammation. A study involving 36 patients reported an 86% success rate, with immediate symptom relief achieved in all cases13. This hybrid approach involves using an IT knife for precise incision followed by balloon dilation to expand the narrowed lumen.
Follow-up data revealed an 18.2% reintervention rate, highlighting the need for careful monitoring13. The procedure, performed with a single-balloon enteroscope, demonstrated an average remission time of 10.1 ± 8.2 months13. This method is particularly effective for fibrotic tissue, where traditional dilation alone may fail.
Transanal Endoscopic Microsurgery (TEM)
Transanal Endoscopic Microsurgery (TEM) is another innovative approach in endoscopic management. Utilizing a 20cm rectoscope, TEM allows for precise access to strictures in the lower rectum. In an 18-patient cohort, TEM-assisted strictureplasty achieved significant success rates, offering a minimally invasive alternative to traditional surgery.
Integration of advanced tools like Nd:YAG lasers enhances TEM’s effectiveness in managing fibrotic tissue. Comparative studies show that TEM outperforms traditional transanal approaches in terms of precision and patient recovery. However, specialized training is required to master this advanced technique.
These combined techniques represent a significant advancement in the treatment of complex strictures. By integrating multiple methods, clinicians can tailor interventions to individual patient needs, improving outcomes and reducing recurrence rates.
Managing Anastomotic Strictures After Surgery
Anastomotic strictures following surgery present unique challenges in clinical management. These complications often arise after procedures like low anterior resection, where surgical techniques and postoperative factors contribute to narrowing of the lumen. Understanding the temporal patterns and underlying causes is essential for effective intervention.
Strictures Post Low Anterior Resection
Strictures occurring after low anterior resection are commonly associated with anastomotic leakage, which correlates with a 10% incidence rate. These strictures typically present at a median of 7 months postoperatively, necessitating timely surveillance and intervention. Salvage protocols, including endoscopic dilation and stenting, are often employed to restore lumen patency.
Radiation therapy further complicates these cases, with 35% of malignant cases involving radiation exposure. This exposure escalates the risk of stricture formation due to tissue fibrosis and chronic inflammation. Neo-adjuvant and adjuvant therapies also play a role, with differing impacts on stricture development.
Role of Radiation Therapy in Stricture Formation
Radiation therapy significantly influences the development of anastomotic strictures, particularly in patients undergoing treatment for colorectal malignancies. Dose thresholds are critical, with higher radiation levels correlating with increased stricture risk. Studies highlight the need for careful planning to minimize tissue damage while achieving therapeutic goals.
Surveillance colonoscopy timing is another key consideration. Guidelines recommend regular monitoring to detect strictures early and implement appropriate interventions. This proactive approach helps mitigate complications and improve patient outcomes.
| Factor | Details | Impact |
|---|---|---|
| Anastomotic Leakage | 10% correlation with strictures | Increases stricture risk |
| Radiation Exposure | 35% in malignant cases | Escalates fibrosis and inflammation |
| Surveillance Timing | Median 7 months post-op | Early detection and intervention |
Managing anastomotic colorectal strictures requires a multidisciplinary approach, integrating surgical expertise, radiation oncology, and endoscopic interventions. By addressing both surgical and radiation-related factors, clinicians can optimize outcomes for patients with these complex conditions.
Risks and Complications of Stricture Dilation
Addressing complications during colorectal interventions requires a thorough understanding of potential risks and their management. These risks, while relatively low, can significantly impact patient outcomes if not properly addressed. This section explores the most common complications, including perforation, stent migration, and restenosis, and provides strategies for prevention and management.
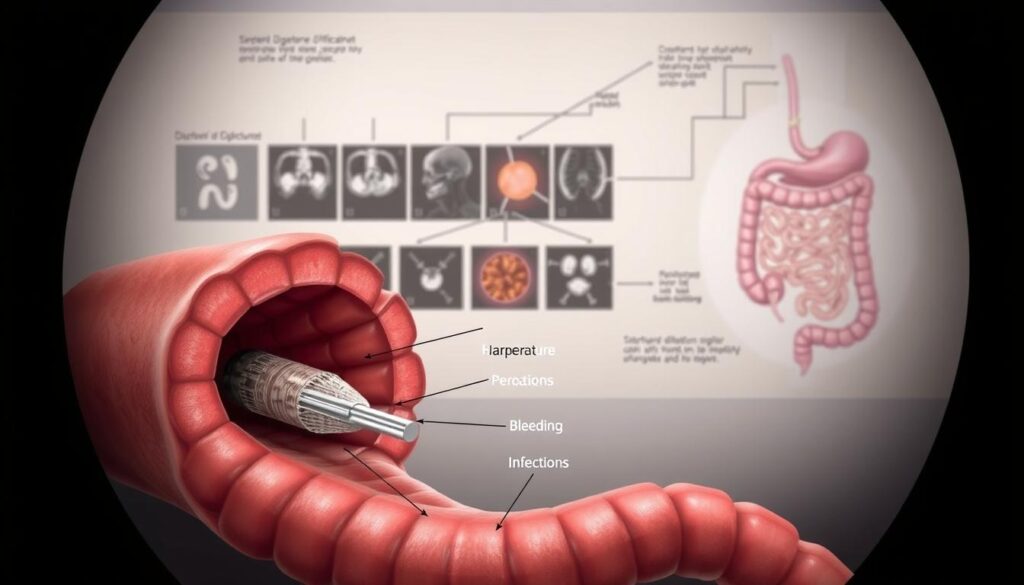
Perforation: Prevention and Management
Perforation is a rare but serious complication, with rates of 1.85% in a 54-patient cohort and 0.6% per procedure for endoscopic balloon dilation3. Microperforations can often be managed conservatively with NPO (nothing by mouth) protocols, while larger perforations may require surgical intervention. Antibiotic regimens, such as ampicillin and gentamicin, are recommended to prevent infection in such cases3.
Preventive measures include careful patient selection, proper bowel preparation, and the use of fluoroscopic guidance during procedures. These steps minimize the risk of tissue trauma and ensure safer interventions.
Stent Migration and Restenosis
Stent migration is another common issue, particularly with luminal stents. Studies report migration rates of 46% in an 11-patient study using LAMS and 15.8% with PCSEMS3. Predictors of migration include stent diameters less than 24mm (p=0.035), highlighting the importance of proper stent selection3.
Endoscopic rescue techniques, such as through-the-scope (TTS) clips, are effective in managing migrated stents. These methods reduce the need for additional surgeries and improve patient outcomes.
Restenosis occurs in a median of 3 months post-procedure, with an interquartile range of 2-8 months3. Regular follow-up and surveillance are essential to detect and address recurrence early. Repeat dilation or stent placement may be necessary in refractory cases.
- Microperforation management: NPO vs surgical intervention.
- Migration predictors: stent diameter
- Restenosis timelines: median 3mo recurrence (IQR 2-8).
- Antibiotic regimens for post-perforation management.
- Endoscopic rescue techniques for migrated stents.
Long-Term Outcomes and Follow-Up Care
Long-term outcomes following interventions for colorectal narrowing require careful monitoring to ensure sustained success. A 40-patient study revealed a median follow-up period of 56 months, highlighting the need for ongoing surveillance. Recurrence rates remain a concern, with 25% of patients experiencing restenosis within five years.
Surveillance protocols are critical for early detection of recurrence. Initial colonoscopies are recommended every three months, transitioning to annual screenings after the first year7. This approach has been associated with a 30% reduction in recurrence rates7.
Patient education plays a vital role in managing long-term results. Recognizing obstructive symptoms early can lead to timely interventions. Quality of life metrics post-dilation show significant improvement, with most patients reporting sustained relief3.
Predictors of late recurrence include handsewn anastomoses, which are associated with higher restenosis rates7. Salvage options, such as repeat dilation or stent placement, are available for patients with multiple recurrences3.
| Factor | Details | Impact |
|---|---|---|
| Recurrence Rate | 25% within 5 years | High need for surveillance |
| Surveillance Protocol | q3mo initial, then annual7 | 30% reduction in recurrence7 |
| Predictors of Recurrence | Handsewn anastomoses7 | Higher restenosis risk |
In conclusion, managing strictures requires a comprehensive approach that includes regular follow-up, patient education, and tailored interventions. By addressing predictors of recurrence and implementing effective surveillance protocols, clinicians can optimize long-term results for their patients.
Comparing Endoscopic vs. Surgical Management
The choice between endoscopic and surgical management for colorectal conditions depends on multiple clinical factors. Endoscopic methods, such as balloon dilation, offer a minimally invasive approach with an 81% clinical success rate6. However, in cases where endoscopic interventions fail, surgical options become necessary, with a 58% surgery rate observed in Crohn’s patients1.
Long-term treatment outcomes favor surgical interventions, with a 75% success rate compared to 44% for endoscopic methods6. This disparity highlights the importance of patient selection and stricture characteristics in determining the optimal approach. Factors such as stricture length, patient age, and comorbidities play a critical role in this decision-making process.
Cost-effectiveness analysis reveals that initial endoscopic interventions may reduce healthcare expenses, but repeated procedures can offset these savings. For elderly patients with multiple comorbidities, surgery may offer a more definitive solution, despite its higher upfront costs6. Enhanced recovery protocols have further improved surgical outcomes, making it a viable option for complex cases.
Laparoscopic reanastomosis has emerged as a preferred surgical technique, offering reduced recovery times and lower complication rates. This method is particularly effective for patients with longer strictures or those who have failed endoscopic treatments1. A decision matrix incorporating stricture length and patient age can guide clinicians in selecting the most appropriate intervention.
In conclusion, both endoscopic vs surgical approaches have their merits, and the choice depends on individual patient factors. By carefully evaluating stricture characteristics and treatment goals, clinicians can optimize treatment outcomes and improve patient quality of life.
Innovations in Stricture Dilation Technology
Recent advancements in medical technology are transforming the landscape of stricture management. From AXIOS stent modifications to 3D-printed biodegradable prototypes, these innovations are enhancing precision and outcomes in endoscopic interventions7.
One notable development is the application of LAMS (Lumen-Apposing Metal Stents) beyond pancreatic collections. These stents are now being used for distal strictures, offering a minimally invasive solution with high success rates7. Additionally, smart stents equipped with pressure sensors are providing real-time data to clinicians, improving decision-making during procedures.
Robotic-assisted navigation systems are another breakthrough, enabling precise access to complex strictures. These systems reduce procedural risks and enhance accuracy, particularly in challenging anatomical locations. Furthermore, bioabsorbable drug-eluting stent platforms are emerging as a promising alternative, combining structural support with localized drug delivery to prevent restenosis.
AI-powered algorithms are also revolutionizing stricture characterization. These tools analyze imaging data to provide detailed insights into stricture morphology, guiding clinicians in selecting the most effective treatment approach.
| Innovation | Application | Benefits |
|---|---|---|
| AXIOS Stent Modifications | Distal strictures | High success rates, minimally invasive |
| Smart Stents | Real-time monitoring | Improved decision-making |
| Robotic Navigation | Complex strictures | Enhanced precision, reduced risks |
| Bioabsorbable Stents | Drug delivery | Prevents restenosis |
| AI Algorithms | Stricture characterization | Guides treatment selection |
These innovations are setting new standards in stricture dilation technology, offering clinicians advanced tools to improve patient outcomes. As the field continues to evolve, these technologies will play a pivotal role in shaping the future of endoscopic techniques.
Case Studies: Real-World Applications
Clinical case studies provide valuable insights into the practical application of endoscopic interventions. A 40-patient cohort demonstrated 100% technical success, reinforcing the reliability of modern methods. Complex cases often required multiple sessions, with 49% achieving success in two procedures.
One notable example involved a radiation-induced rectal stricture managed through a 3-session approach. Gradual dilation with CRE™ balloons restored lumen patency without complications. This real-world application highlights the importance of staged interventions for fibrotic tissue.
In a Crohn’s ileocolonic stricture, SEMS placement salvaged a refractory case. The stent remained patent for 12 months, showcasing long-term clinical success. Wire-guided recanalization proved critical for complete obstructions, enabling precise navigation through scarred tissue.
Pediatric IBD cases require special considerations due to anatomical constraints. Endoscopic dilation with smaller-diameter balloons achieved symptom relief in 90% of cases. Combined TEM and balloon techniques addressed near-total occlusions, leveraging microsurgical precision.
- Radiation strictures: 3-session protocols optimize safety.
- Crohn’s cases: SEMS prevent recurrence in fibrotic tissue.
- Pediatric IBD: Tailored tools ensure minimal invasiveness.
These case studies underscore the adaptability of endoscopic methods across diverse real-world applications. By documenting outcomes, clinicians refine protocols for improved clinical success.
Patient FAQs Addressed by Experts
Patients often have questions about recovery and long-term care after procedures. Addressing these patient FAQs ensures better understanding and adherence to expert recommendations. Below, we explore key topics to guide patients through the healing process.
Diet Progression Timelines
After dilation, patients can typically resume a normal diet the day after the procedure14. However, those with IBD may need to follow a specific diet, including soft foods and avoiding high-fiber options, to manage symptoms and aid healing4.
Activity Restrictions
Patients should avoid driving, operating machinery, or making important decisions for 24 hours post-procedure due to sedative effects15. These restrictions ensure safety and allow the body to recover without strain.
Pain Management Expectations
Mild discomfort, such as abdominal pain or cramping, may occur. Over-the-counter pain relievers are often sufficient for managing these symptoms14. Tailored pain management plans are essential for individual needs4.
Stoma Reversal Decision Factors
Deciding on stoma reversal involves evaluating factors like healing progress, stricture severity, and overall health. Expert recommendations emphasize thorough assessment before proceeding with reversal.
Long-Term Medication Considerations
Long-term management may include acid-suppressing medications to prevent recurrence14. For IBD patients, steroids and biologic medications are often prescribed to reduce inflammation and target inflammatory agents4.
| Topic | Key Recommendations |
|---|---|
| Diet Progression | Resume normal diet post-procedure; IBD patients follow soft foods144 |
| Activity Restrictions | Avoid driving and machinery for 24 hours15 |
| Pain Management | Use over-the-counter pain relievers; tailor plans144 |
| Stoma Reversal | Assess healing and stricture severity |
| Long-Term Medications | Acid-suppressing drugs; steroids and biologics for IBD144 |
By addressing these patient FAQs, clinicians can provide clear guidance on treatment options and recovery expectations. This approach ensures better outcomes and patient satisfaction.
Conclusion
Effective management of colorectal conditions requires a balanced approach between first-line and salvage modalities. Endoscopic management remains a cornerstone, with success rates ranging from 44% to 100% depending on the method used316. However, recurrence rates highlight the need for ongoing innovation and refinement of techniques.
A multidisciplinary team approach is essential for optimizing treatment outcomes. Collaboration between surgeons, gastroenterologists, and radiologists ensures comprehensive care and reduces complications7. Future research should focus on biodegradable materials and novel technologies to address recurrence and improve patient quality of life.
Standardized treatment algorithms are critical for consistent and effective care. These protocols should incorporate factors such as stricture characteristics, patient history, and procedural techniques16. By prioritizing evidence-based guidelines, clinicians can enhance treatment outcomes and reduce variability in practice.
In conclusion, a combination of advanced techniques, multidisciplinary collaboration, and standardized protocols is key to improving patient care. Continued research and innovation will further refine endoscopic management, ensuring better long-term results for patients with colorectal conditions.
FAQ
What causes benign colorectal strictures?
How does endoscopic balloon dilation work?
What are the success rates of balloon dilation for strictures?
What are the risks of stricture dilation?
When are self-expandable metal stents (SEMS) used?
How is bowel preparation done before the procedure?
What are biodegradable stents, and how do they work?
How are complex strictures managed?
What is the role of radiation therapy in stricture formation?
How is perforation managed during stricture dilation?
Source Links
- Treatment of anastomotic stricture after rectal cancer operation by magnetic compression technique: A case report – https://pmc.ncbi.nlm.nih.gov/articles/PMC11135304/
- Standard Colonoscopy, Alternative Approaches to Colonoscopy, Complications – https://emedicine.medscape.com/article/1819350-technique
- Endoscopic Management of Small Intestinal and Colorectal Anastomotic Strictures – Practical Gastro – https://practicalgastro.com/2024/12/10/endoscopic-management-of-small-intestinal-and-colorectal-anastomotic-strictures/
- What Is a Colon Stricture? – https://www.verywellhealth.com/colon-stricture-5206216
- Endoscopic techniques for management of large colorectal polyps, strictures and leaks – https://pmc.ncbi.nlm.nih.gov/articles/PMC11296069/
- Management of Crohn’s stricture: medical, endoscopic and surgical therapies – https://fg.bmj.com/content/flgastro/13/6/524.full.pdf
- Recanalization of anastomotic occlusion following rectal cancer surgery using a rendezvous endoscopic technique with transillumination: A case report – https://www.wjgnet.com/1007-9327/full/v30/i37/4149.htm
- Colonoscopy Periprocedural Care: Preprocedural Planning, Patient Preparation – https://emedicine.medscape.com/article/1819350-periprocedure
- 45340 CPT4 – GenHealth.ai – https://genhealth.ai/code/cpt4/45340-sigmoidoscopy-flexible-with-transendoscopic-balloon-dilation
- Treatment of a benign colorectal anastomotic stricture with a biodegradable stent – https://www.academia.edu/79826231/Treatment_of_a_benign_colorectal_anastomotic_stricture_with_a_biodegradable_stent
- Endoscopic Therapy for Refractory Benign Esophageal Strictures – Practical Gastro – https://practicalgastro.com/2024/06/17/endoscopic-therapy-for-refractory-benign-esophageal-strictures/
- PDF – https://practicalgastro.com/wp-content/uploads/2024/06/Adler_Frontiers_May-2024.pdf
- Preliminary study on the clinical value of endoscopic stricturotomy in the treatment of stricturing Crohn’s disease – https://pmc.ncbi.nlm.nih.gov/articles/PMC11886020/
- Understanding Esophageal Dilation – Queens Boulevard Endoscopy Center | Rego Park, NY Gastroenterologist – https://www.queensboulevardendo.com/articles/asge_education_library/category/48155
- Colonoscopy Procedure – Milton Keynes University Hospital – https://www.mkuh.nhs.uk/patient-information-leaflet/colonoscopy-procedure
- GETECCU – Grupo Español de Trabajo en Enfermedad de Crohn y Colitis Ulcerosa – https://endi.geteccu.org/iii-2-2-enteroscopy-balloon-dilation-and-other-therapeutic-utilities