Key Takeaways
- Understanding the Fundamentals of ERCP
- Preparing for Your ERCP Appointment
- ERCP Technique for Bile Duct Stone Removal
- The ERCP Procedure: Steps and Tools Involved
Endoscopic retrograde cholangiopancreatography (ERCP) is a critical procedure in managing biliary conditions. It combines upper gastrointestinal endoscopy and fluoroscopy to diagnose and treat disorders of the bile duct and pancreatic systems. This method allows for precise visualization and intervention, making it a cornerstone in modern gastroenterology.
The use of an endoscope and contrast dye enables clinicians to identify obstructions, such as gallstones, with high accuracy. ERCP not only aids in diagnosis but also facilitates therapeutic interventions, reducing the need for invasive surgeries. Its technical success rate is 83.3%, with a similar clinical success rate observed in patient outcomes1.
Understanding the anatomy of the bile duct is essential for minimizing risks and ensuring effective treatment. Adverse events, such as post-procedure pancreatitis, occur in 16.7% of cases, highlighting the importance of skilled execution1. This procedure remains a vital tool for healthcare professionals addressing complex biliary disorders.
Key Takeaways
- ERCP combines endoscopy and fluoroscopy for precise diagnosis and treatment.
- It has a technical and clinical success rate of 83.3%1.
- The procedure minimizes the need for invasive surgeries.
- Understanding bile duct anatomy is crucial for reducing risks.
- Adverse events, such as pancreatitis, occur in 16.7% of cases1.
Understanding the Fundamentals of ERCP
Endoscopic retrograde cholangiopancreatography (ERCP) integrates endoscopy and fluoroscopy to address biliary and pancreatic duct abnormalities. This combined approach allows clinicians to diagnose and treat conditions affecting these systems with precision2.
What is ERCP?
ERCP is a minimally invasive procedure that uses an endoscope and X-ray imaging to visualize the bile and pancreatic ducts. A contrast dye is administered through a tube to highlight blockages or abnormalities, enabling targeted interventions3.
The Role of Endoscopy and Fluoroscopy
During the procedure, an endoscope is inserted through the mouth to reach the duct system. Fluoroscopy provides real-time imaging, guiding the clinician in identifying and resolving issues. This dual approach minimizes the need for invasive surgeries4.
Potential complications include pancreatitis, infection, or perforation of the duct. Symptoms such as abdominal pain or fever may occur post-procedure, requiring careful monitoring2. Proper patient management, including fasting and sedation, ensures safety and effectiveness3.
The anatomy of the bile and pancreatic ducts plays a pivotal role in understanding biliary and pancreatic disorders. These structures form a complex network essential for digestion and waste elimination. Detailed knowledge of their morphology is critical for accurate diagnosis and effective treatment.
Overview of Bile Duct Structure
The bile duct system consists of intrahepatic and extrahepatic components. Intrahepatic ducts collect bile from the liver, while the common bile duct transports it to the duodenum. This system is often affected by obstructions, such as gallstones, which can lead to complications like jaundice or cholangitis5.
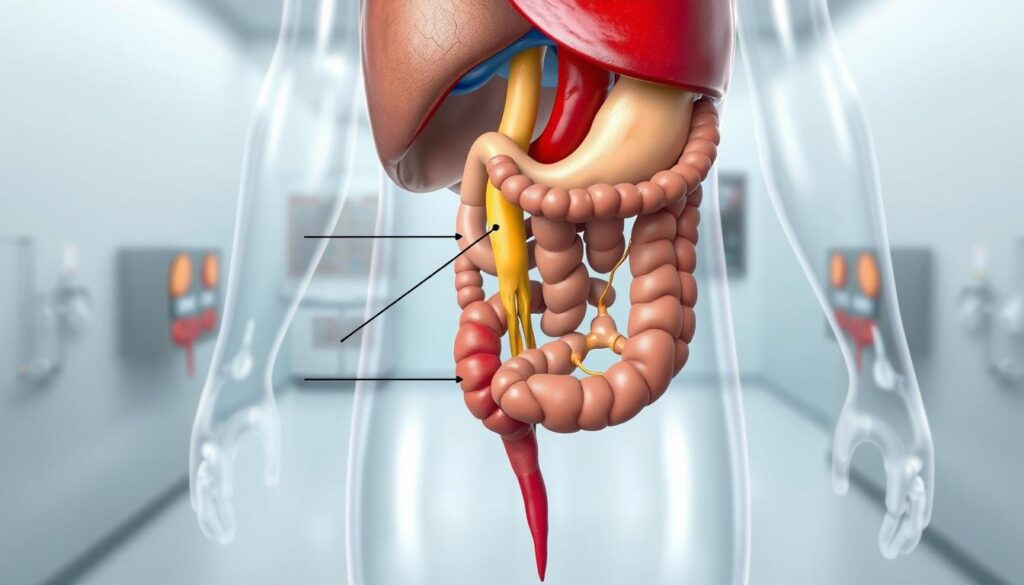
Understanding the Pancreatic Ducts
The pancreatic duct runs through the pancreas, merging with the common bile duct at the ampulla of Vater. This junction is a common site for blockages, often caused by gallstones or strictures. Accurate imaging of this area is crucial for planning interventions6.
Gallstones are a frequent cause of obstruction in both the bile and pancreatic ducts. They can lead to severe symptoms, including abdominal pain and pancreatitis. Understanding the anatomical details of these ducts helps clinicians identify and resolve such issues effectively5.
- The bile duct system includes intrahepatic and extrahepatic components.
- The pancreatic duct merges with the common bile duct at the ampulla of Vater.
- Gallstones are a common cause of obstruction in these ducts.
- Anatomical knowledge aids in accurate diagnosis and treatment planning.
Preparing for Your ERCP Appointment
Proper preparation is essential for a successful ERCP procedure. Patients must follow specific guidelines to ensure safety and effectiveness. This includes fasting, medication adjustments, and a thorough review of medical history.
Pre-Procedure Guidelines and Medical History
Before the procedure, patients are advised to fast for at least 6 hours to ensure an empty stomach. Small sips of water are allowed up to 2 hours before the appointment7. A comprehensive review of medical history is conducted to identify potential contraindications, such as allergies or clotting disorders8.
Certain medicines, particularly those affecting blood clotting, must be managed prior to the procedure. This reduces the risk of complications like bleeding9. Patients should inform their healthcare provider about all medications they are taking.
Dietary Restrictions and Medication Adjustments
Dietary restrictions are crucial for procedural safety. Patients should avoid solid foods and adhere to a liquid diet for the specified time frame7. Antibiotics are typically administered 1 hour before the procedure to minimize the risk of infection8.
Administrative steps, such as arranging hospital admission details and post-procedural care, are also important. Patients should plan for an escort to assist them after the procedure, as sedation may impair their ability to drive9.
ERCP Technique for Bile Duct Stone Removal
Addressing obstructions in the biliary system requires a precise and effective approach. This method combines diagnostic imaging with therapeutic interventions to resolve blockages and alleviate symptoms. It is particularly useful when gallstones cause significant complications, such as pancreatitis or jaundice10.
Diagnostic vs. Therapeutic Purposes
The procedure serves dual roles: identifying the issue and providing immediate treatment. Diagnostic imaging helps locate obstructions in the pancreatic duct or gallbladder. Therapeutic interventions, such as stone extraction, are performed during the same session11.
This approach minimizes the need for multiple procedures, reducing patient discomfort and recovery time. It is especially beneficial for individuals experiencing severe pain or complications from gallstones10.
When and Why This Procedure is Recommended
The procedure is recommended when noninvasive tests fail to resolve the problem. It is often used for patients with gallstones obstructing the bile duct or those at risk of pancreatitis11.
Anesthesia and sedatives are administered to ensure patient comfort and procedural precision. This allows the clinician to navigate the endoscope through the duodenum and administer contrast dye for clear imaging10.
In cases where stones are irretrievable, stenting may be required to restore bile flow. This highlights the importance of thorough patient assessment before proceeding11.
The ERCP Procedure: Steps and Tools Involved
The ERCP process involves a series of carefully orchestrated steps to ensure accurate diagnosis and effective treatment. This minimally invasive approach combines advanced imaging and therapeutic techniques to address issues in the biliary and pancreatic systems12.
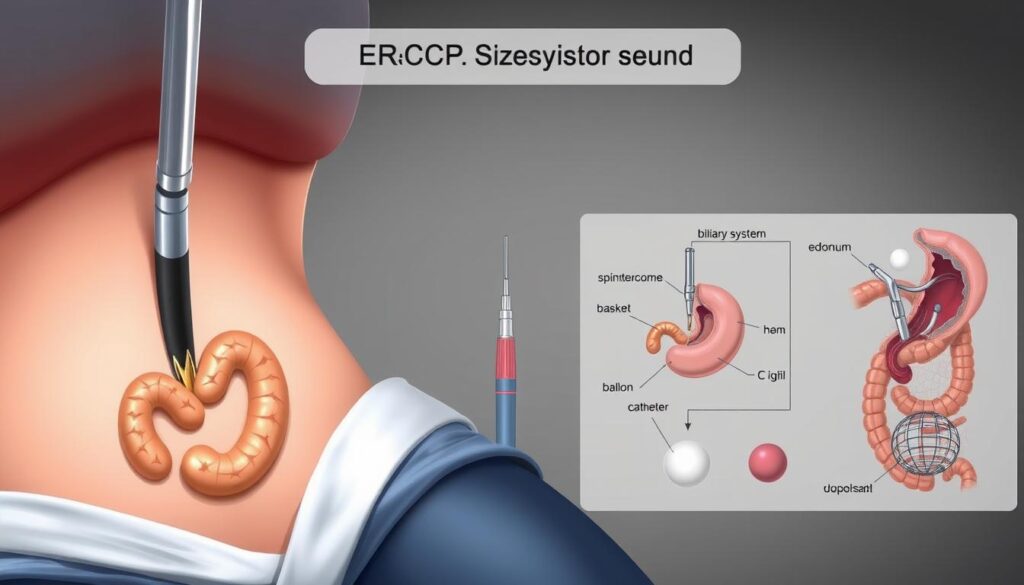
Administration of Sedatives and Anesthesia
Before the procedure begins, patients are administered sedatives and anesthesia to ensure comfort and minimize movement. An IV line is placed to deliver these medications, which help relax the patient and reduce discomfort during the process13.
Proper sedation is critical to the success of the procedure, as it allows the clinician to navigate the endoscope with precision. Patients are monitored closely to ensure their safety throughout12.
Step-by-Step Endoscope Navigation
The endoscope is carefully guided through the esophagus, stomach, and into the duodenum. Air is introduced to expand these areas, providing better visibility for the clinician14.
This step requires skill and precision to avoid complications such as perforation or injury to the gastrointestinal tract. Real-time imaging ensures accurate navigation13.
Use of Contrast Dye and Fluoroscopy
Once the endoscope is in position, a contrast dye is injected into the ducts. This dye highlights any blockages or abnormalities, allowing for detailed imaging under fluoroscopy12.
Fluoroscopy provides real-time X-ray images, enabling the clinician to identify and address issues immediately. This combination of tools ensures a thorough and effective procedure14.
“The precision of ERCP lies in its ability to combine diagnostic imaging with therapeutic interventions, all within a single procedure.”
| Tool | Purpose |
|---|---|
| Endoscope | Visualizes and navigates the gastrointestinal tract |
| Contrast Dye | Highlights blockages or abnormalities in the ducts |
| Fluoroscopy | Provides real-time imaging for accurate diagnosis and treatment |
Post-ERCP: Recovery, Risks, and What to Expect
Post-procedure care is a critical component of ensuring successful outcomes after an endoscopic intervention. Patients are closely monitored in a hospital setting to manage pain and detect any complications early15.
https://www.youtube.com/watch?v=iEyqdQ_Iddc
Immediate Post-Procedure Recovery Guidelines
After the procedure, patients are observed until the effects of anesthesia wear off, typically within 45-60 minutes16. Vital signs, including blood pressure and heart rate, are monitored to ensure stability. Mild discomfort in the throat or stomach is common and usually resolves quickly.
Patients are advised not to drive for 24 hours due to lingering sedation effects. A liquid diet is often recommended initially, with a gradual return to solid foods as tolerated15.
Recognizing and Managing Potential Complications
While most patients recover without issues, some may experience complications such as pancreatitis or infection. Symptoms like severe abdominal pain, fever, or difficulty swallowing should prompt immediate medical attention16.
In rare cases, perforation of the intestine or significant bleeding may occur, requiring further intervention. Patients are educated on recognizing these signs to ensure timely treatment15.
| Recovery Step | Details |
|---|---|
| Monitoring | Vital signs and pain levels are checked regularly in the hospital. |
| Dietary Adjustments | Start with liquids, then progress to soft foods as tolerated. |
| Activity Restrictions | Avoid driving and strenuous activities for 24 hours. |
| Follow-Up | Schedule a follow-up appointment to assess recovery and address concerns. |
Proper post-procedure care minimizes risks and promotes a smooth recovery. Patients should follow all guidelines provided by their healthcare team to ensure optimal outcomes16.
Conclusion
Managing biliary and pancreatic conditions requires a structured, evidence-based approach. This method integrates diagnostic testing with therapeutic interventions, ensuring precise and effective treatment for patients. Understanding the anatomy of the pancreatic duct and gallbladder is crucial for minimizing risks and achieving optimal outcomes17.
Healthcare professionals must coordinate closely before, during, and after the procedure to ensure patient safety. Proper preparation, including fasting and medication adjustments, is essential for success. Post-procedural care, such as monitoring for complications like pancreatitis, further enhances recovery18.
This comprehensive approach highlights the importance of skilled execution and evidence-based practice. By addressing biliary obstructions effectively, clinicians can improve patient health and reduce the need for invasive surgeries17.
FAQ
What is endoscopic retrograde cholangiopancreatography (ERCP)?
Endoscopic retrograde cholangiopancreatography (ERCP) is a medical procedure used to diagnose and treat conditions affecting the bile and pancreatic ducts. It combines endoscopy and fluoroscopy to visualize and address issues like gallstones, blockages, or tumors.
How does endoscopy and fluoroscopy work in ERCP?
During ERCP, an endoscope is inserted through the mouth to reach the duodenum. Fluoroscopy, a type of X-ray imaging, is used to guide the endoscope and visualize the bile and pancreatic ducts after injecting a contrast dye.
What are the key components of the bile and pancreatic ducts?
The bile duct carries bile from the liver and gallbladder to the small intestine, while the pancreatic duct transports digestive enzymes from the pancreas. Both ducts join at the duodenum, playing a crucial role in digestion.
How should I prepare for an ERCP procedure?
Preparation includes fasting for 6-8 hours before the procedure, adjusting medications as advised by your doctor, and providing a detailed medical history. Inform your healthcare provider about any allergies or existing conditions.
What are the differences between diagnostic and therapeutic ERCP?
Diagnostic ERCP is used to identify issues like blockages or tumors, while therapeutic ERCP involves treatments such as stone removal, stent placement, or duct dilation to address the identified problems.
What steps are involved in the ERCP procedure?
The procedure begins with sedation or anesthesia. An endoscope is guided to the duodenum, and contrast dye is injected to highlight the ducts. Fluoroscopy helps locate and treat issues like gallstones or strictures.
What should I expect during recovery after ERCP?
Recovery typically involves monitoring for a few hours post-procedure. Mild throat discomfort or bloating may occur. Follow dietary guidelines and watch for signs of complications like severe pain or fever.
What are the potential risks or complications of ERCP?
Risks include pancreatitis, infection, bleeding, or perforation. Symptoms like persistent pain, fever, or jaundice should be reported immediately to your healthcare provider.
Source Links
- Endoscopic retrograde cholangiopancreatography combined with extracorporeal shock wave lithotripsy for the removal of large gallbladder stones: a pilot study – BMC Gastroenterology – https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-025-03590-y
- Endoscopic Retrograde Cholangiopancreatography (ERCP) – https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/endoscopic-retrograde-cholangiopancreatography-ercp
- Bumrungrad International Hospital – https://www.bumrungrad.com/en/treatments/ercp-endoscopic-retrograde-cholangio-pancreatography
- Endoscopic management of bile duct stones – https://www.uptodate.com/contents/endoscopic-management-of-bile-duct-stones
- ERCP Procedure Overview | The Iowa Clinic – https://www.iowaclinic.com/specialties/digestive-health/endoscopy/tests-procedures/endoscopic-retrograde-cholangiopancreatography-ercp/
- Percutaneous Transhepatic Cholangiography – StatPearls – https://www.ncbi.nlm.nih.gov/books/NBK493190/
- ERCP (endoscopic retrograde cholangio pancreatography) – Having an ERCP – https://www.guysandstthomas.nhs.uk/health-information/ercp-endoscopic-retrograde-cholangio-pancreatography/having-ercp
- Endoscopic Retrograde Cholangiopancreatography (ERCP) | Bangkok Hospital – https://www.bangkokhospital.com/en/content/endoscopic-retrograde-cholangiopancreatography
- Endoscopic Retrograde Cholangiopancreatography (ERCP) – https://www.materprivate.ie/our-services/digestive-diseases/endoscopic-retrograde-cholangiopancreatography-(ercp)
- Repeat ERCP versus Common Bile Duct Exploration for Failed Stone Clearance: A Prospective Randomized Study – https://clinmedjournals.org/articles/ijsrp/international-journal-of-surgery-research-and-practice-ijsrp-11-171.php?jid=ijsrp
- Bile Duct Stones Removal Singapore – ERCP Procedure Singapore – https://www.leesurgery.com.sg/service/bile-duct-stones/
- Diagnosing Digestive Diseases With ERCP – https://www.webmd.com/digestive-disorders/digestive-diseases-ercp
- ERCP – https://www.apollohospitals.com/diagnostics-investigations/ercp/
- Cary Gastroenterology Associates | What is Endoscopic Retrograde… – https://www.carygastro.com/blog/what-is-endoscopic-retrograde-cholangiopancreatography-ercp
- Endoscopic Retrograde Cholangiopancreatography (ERCP) in Denver – https://gicolorado.com/endoscopic-retrograde-cholangiopancreatography-ercp-denver-co/
- Endoscopic Retrograde Cholangiopancreatography (ERCP) in Oklahoma – https://adultgastro.com/endoscopic-retrograde-cholangiopancreatography-ercp-tulsa-ok/
- Surgical strategies for challenging common bile duct stones in the endoscopic era: A comprehensive review of current evidence – https://pmc.ncbi.nlm.nih.gov/articles/PMC11212516/
- Clinical application of ERCP concurrent laparoscopic cholecystectomy in the treatment of cholecystolithiasis complicated with extrahepatic bile duct stones – https://pmc.ncbi.nlm.nih.gov/articles/PMC11128888/