In the field of gastroenterology, the treatment of lesions has evolved significantly with the advent of minimally invasive techniques. Endoscopic mucosal resection and endoscopic submucosal dissection are two prominent methods used for the removal of abnormal tissue. These procedures have become the preferred treatment modalities due to their precision and reduced recovery times.
Endoscopic mucosal resection involves the removal of lesions from the mucosal layer, while endoscopic submucosal dissection allows for complete lesion removal by dissecting the submucosal layer. Studies have shown that submucosal dissection techniques result in higher en bloc resection rates, which significantly influence recurrence outcomes1.
Understanding the differences between these techniques is crucial for making informed therapeutic decisions. Both methods have their unique advantages and limitations, which will be explored in this comparative analysis.
Key Takeaways
- Endoscopic mucosal resection and endoscopic submucosal dissection are minimally invasive techniques.
- Submucosal dissection allows for complete lesion removal, reducing recurrence rates.
- En bloc resection rates are higher with submucosal dissection techniques.
- Both methods have unique advantages and limitations.
- Informed therapeutic decisions require a thorough understanding of both techniques.
Introduction and Clinical Relevance
The management of abnormal tissue in the gastrointestinal tract has seen significant advancements in recent years. Minimally invasive techniques, such as endoscopic mucosal resection, have become pivotal in modern gastroenterology. These methods offer precision and reduced recovery times, making them the preferred choice for many practitioners.
Studies, including the RESECT-COLON trial, highlight the importance of these techniques in achieving effective polyp removal. Data shows that up to 15% of colorectal polyps are not suitable for conventional polypectomy, emphasizing the need for advanced endoscopic methods2.
Overview of Abnormal Tissue Removal
Endoscopic techniques play a critical role in removing abnormal tissue from the mucosal layer. These procedures are particularly effective for lesions that are challenging to address with traditional methods. For instance, mucosal resection allows for the removal of lesions with minimal disruption to surrounding tissue.
However, challenges such as recurrence rates remain a concern. Piecemeal resection, often used in complex cases, has been associated with higher recurrence rates compared to en bloc removal3. This underscores the importance of selecting the appropriate technique based on lesion characteristics.
Importance in Gastroenterology
The clinical relevance of these techniques extends beyond immediate treatment outcomes. High-quality patient assessment is essential to minimize recurrence and ensure long-term success. Surveillance protocols are often adjusted based on the recurrence rate observed post-procedure.
“The choice of endoscopic technique significantly impacts patient outcomes, particularly in reducing recurrence rates.”
Data from Kaiser Permanente reveals that recurrence rates following piecemeal resection can range from 10% to 23.5%, while en bloc resection offers rates as low as 0.9%2. This highlights the need for meticulous technique selection and execution.
| Technique | En Bloc Resection Rate | Recurrence Rate |
|---|---|---|
| Endoscopic Mucosal Resection | 44.5% – 63% | 7.4% – 17% |
| Endoscopic Submucosal Dissection | 87.9% – 96% | 0.9% – 2% |
In conclusion, the clinical relevance of endoscopic techniques in gastroenterology cannot be overstated. These methods not only improve patient outcomes but also reduce the burden of recurrence, making them indispensable in modern practice.
Understanding Endoscopic Mucosal Resection (EMR)
Endoscopic mucosal resection (EMR) has emerged as a cornerstone in modern gastroenterology for treating abnormal tissue. This minimally invasive technique allows for precise removal of lesions from the mucosal layer, offering reduced recovery times and improved patient outcomes. The procedure involves several critical steps, including submucosal injection and snaring techniques, which ensure effective lesion removal4.
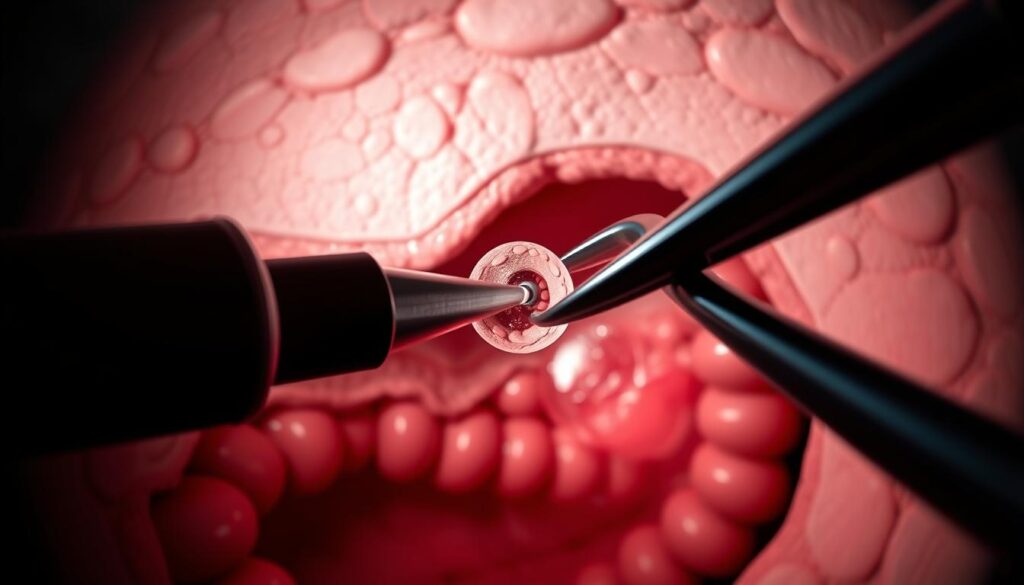
Technique Fundamentals and Procedure Steps
The EMR process begins with a submucosal injection, which lifts the lesion from the underlying tissue. This step is crucial for creating a safe dissection plane. A snare is then used to remove the lesion, either in one piece (en bloc) or in multiple fragments (piecemeal). En bloc resection is preferred for its lower recurrence rates, but piecemeal resection is often necessary for larger lesions5.
Challenges arise when dealing with large lesions, as complete removal becomes more complex. The learning curve for EMR is steep, requiring significant expertise to achieve optimal outcomes. Studies show that procedure times average around 14.5 minutes, with recurrence rates as low as 5.1% when performed by skilled endoscopists6.
Clinical Outcomes and Recurrence Rates
Clinical outcomes of EMR are influenced by the technique used and the size of the lesion. En bloc resection rates for smaller lesions (10–19 mm) are significantly higher compared to larger ones (>20 mm). Recurrence rates are also lower for en bloc resections, highlighting the importance of technique selection4.
Piecemeal resection, while effective for complex cases, is associated with higher recurrence rates. This underscores the need for meticulous follow-up and surveillance protocols. The table below provides a comparative analysis of EMR outcomes based on resection type and lesion size.
| Resection Type | Lesion Size | En Bloc Rate | Recurrence Rate |
|---|---|---|---|
| En Bloc | 10–19 mm | 93.2% | 0.9% |
| Piecemeal | >20 mm | 54.0% | 19.3% |
In conclusion, EMR remains a vital tool in gastroenterology for lesion removal. Its success depends on technical precision, lesion characteristics, and the expertise of the endoscopist. By adhering to high standards, practitioners can minimize recurrence and improve patient outcomes.
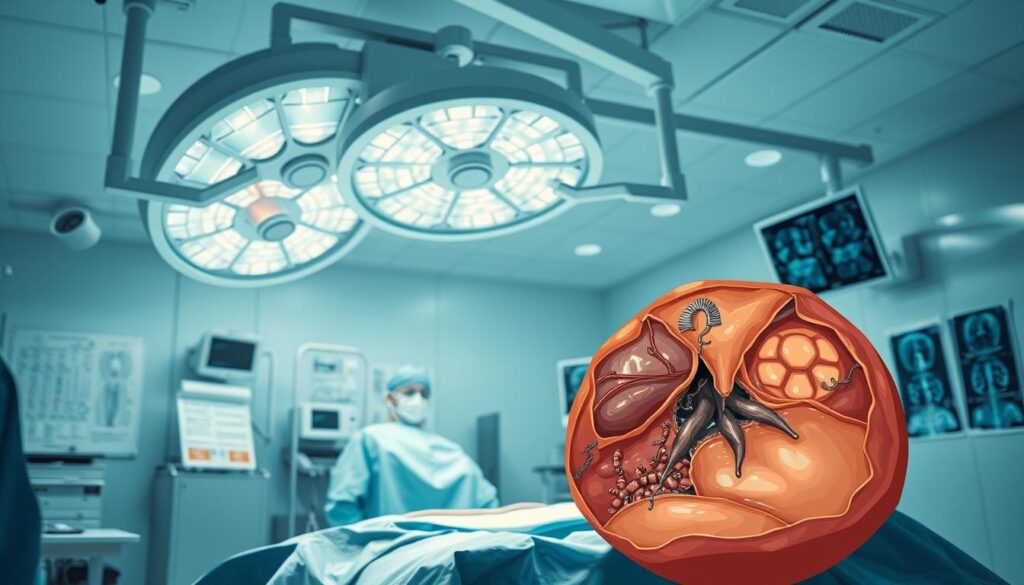
Exploring Endoscopic Submucosal Dissection (ESD)
Endoscopic submucosal dissection (ESD) represents a significant advancement in the management of gastrointestinal lesions. This technique allows for precise removal of abnormal tissue, particularly in cases where early cancer invasion is suspected. Unlike conventional methods, ESD enables complete lesion removal in one piece, reducing the risk of leaving tumor cells behind7.
Procedure Overview and En Bloc Resection
The ESD process involves several critical steps. First, a submucosal injection is administered to lift the lesion from the underlying tissue. This is followed by a circumferential incision and careful dissection of the submucosal layer. The goal is to achieve en bloc resection, which ensures clear margins and aids in accurate cancer staging8.
Studies show that ESD achieves an en bloc resection rate of 81.9%, significantly higher than other methods8. This precision is particularly beneficial for lesions larger than 4 cm, where the odds of achieving a resection speed greater than 9 cm²/hr are 9.16 times higher8.
Safety Considerations and Adverse Events
While ESD offers superior outcomes, it comes with increased procedure times and higher costs. The median procedure time is 81 minutes, with longer durations for larger lesions8. Additionally, adverse events such as delayed perforations (1%) and bleeding (1.3%) are more common compared to other techniques8.
In cases of non-curative resection, additional surgery may be required in 5% of cases8. Despite these challenges, ESD remains a vital tool for managing complex lesions, particularly those with high suspicion for early cancer invasion.
| Aspect | ESD | Other Techniques |
|---|---|---|
| En Bloc Resection Rate | 81.9% | 44.5% – 63% |
| Procedure Time | 81 minutes | 14.5 minutes |
| Adverse Events | 1% – 1.3% | 0.5% – 0.9% |
| Additional Surgery | 5% | 2% – 3% |
Comparing EMR vs ESD for Large Colon Polyps
Advancements in endoscopic techniques have revolutionized the management of gastrointestinal lesions, offering precise and minimally invasive solutions. These methods have become essential tools for clinicians, providing effective treatment options with reduced recovery times and improved patient outcomes.
Efficacy, Complete Resection, and Recurrence
When comparing the two primary techniques, significant differences emerge in efficacy and recurrence rates. One method achieves an en bloc resection rate of 96.6%, while the other reaches only 10.4%9. This disparity directly impacts recurrence rates, with one technique showing a recurrence rate of 0.6% compared to 5.1% for the other9.
Guidelines recommend selecting the technique based on lesion characteristics and patient condition. For larger lesions, the higher en bloc resection rate of one method makes it the preferred choice1.
Patient Outcomes and Quality of Life
Patient outcomes vary significantly between the two techniques. One method has a higher rate of adverse events at 35.6%, compared to 24.5% for the other9. However, the lower recurrence rate of the former contributes to better long-term quality of life.
Procedure times also differ, with one technique averaging 47 minutes and the other 14.5 minutes9. This impacts healthcare utilization and patient comfort during the procedure.
- En bloc resection rates are significantly higher with one technique, reducing recurrence risks.
- Adverse events are more common with the method offering higher en bloc rates.
- Procedure time is longer for the technique with superior outcomes.
- Guidelines emphasize lesion size and patient condition in technique selection.
In conclusion, the choice between these techniques depends on balancing efficacy, safety, and patient outcomes. Clinicians must consider lesion characteristics and follow established guidelines to optimize results.
Surgical Outcomes, Recurrence, and Adverse Events
The evaluation of surgical outcomes in gastrointestinal procedures has become a critical focus in modern medical practice. Understanding the risks and benefits of endoscopic techniques is essential for optimizing patient care. Recent studies have highlighted the importance of minimizing adverse events in lesion removal procedures.
Analysis of Complication Rates
Complication rates vary significantly between endoscopic techniques. Data from the RESECT-COLON trial indicates that adverse events such as perforation occur in 1% of cases with one method, compared to 0.5% with another10. Post-polypectomy syndromes, including bleeding and delayed perforation, are also more prevalent with certain techniques11.
Recurrence rates are another critical factor. Complete resection reduces recurrence to 0.4%, while incomplete resection increases it to 2.7%11. Thorough assessment protocols are essential to mitigate these risks and ensure optimal outcomes.
Discussion on Post-Polypectomy Syndromes
Post-polypectomy syndromes, such as bleeding and delayed perforation, are significant concerns. Studies show that these complications occur in 1.3% of cases with one technique, compared to 0.9% with another10. Early detection and intervention are crucial to managing these adverse events effectively.
Risk factors include lesion size and location. Larger lesions in the rectosigmoid region have a higher risk of complications, with an odds ratio of 3.1910. Proper patient selection and technique choice are vital to minimizing these risks.
| Technique | Perforation Rate | Bleeding Rate | Recurrence Rate |
|---|---|---|---|
| Technique A | 1% | 1.3% | 0.4% |
| Technique B | 0.5% | 0.9% | 2.7% |
In conclusion, the assessment of surgical outcomes and adverse events is essential for optimizing patient care. By understanding the risks and benefits of each technique, clinicians can make informed decisions that improve long-term outcomes.
Procedure Time, Costs, and Healthcare Utilization
The efficiency and cost-effectiveness of endoscopic techniques play a pivotal role in modern gastroenterology. These factors influence not only patient outcomes but also the broader healthcare system. Understanding the balance between time investment, resource allocation, and long-term benefits is essential for optimizing clinical practice.
Time Investment and Resource Allocation
Endoscopic procedures vary significantly in duration. Studies show that one technique averages 47 minutes, while another takes only 14.5 minutes12. This difference impacts resource allocation, including staffing and equipment utilization.
Longer procedure times often require more skilled endoscopists and specialized tools. However, the reduced recurrence rates associated with these techniques can offset the initial time investment13.
Cost Analysis and Long-Term Benefits
The cost of endoscopic techniques is influenced by procedure complexity and recurrence rates. One method, despite higher initial costs, offers long-term savings by minimizing the need for repeat interventions12.
Economic evaluations highlight that lower recurrence rates translate to fewer follow-up colonoscopies and reduced healthcare expenditures13. This makes certain techniques more cost-effective over time.
“The long-term benefits of advanced endoscopic techniques often justify their higher initial costs, particularly in reducing recurrence and healthcare utilization.”
Healthcare systems must balance these factors to ensure optimal patient outcomes. The table below compares key metrics for two primary techniques.
| Technique | Procedure Time | Initial Cost | Recurrence Rate |
|---|---|---|---|
| Technique A | 47 minutes | $5,000 | 0.6% |
| Technique B | 14.5 minutes | $3,000 | 5.1% |
In conclusion, the choice of endoscopic technique involves careful consideration of time, cost, and long-term outcomes. By prioritizing these factors, healthcare providers can deliver effective and sustainable care.
Endoscopist Training and Skill Development
Mastering endoscopic techniques requires a structured approach to training and skill development. The complexity of procedures like polypectomy for adenomas and colorectal polyps demands rigorous education and hands-on practice. Training programs often emphasize mentorship and progressive case selection to ensure competency14.
Training Requirements and Learning Curve
The learning curve for advanced endoscopic techniques is steep. Trainees are recommended to complete a minimum of 1,000 esophagogastroduodenoscopies (EGDs) and 500 colonoscopies before initiating ESD training14. Additionally, 30 ex vivo procedures are suggested to build foundational skills14.
Early training phases often involve higher risks, such as perforation, which occurs in 13.8% of cases pre-observership14. However, structured training reduces these risks significantly, with no perforations observed post-observership14.
Advanced Endoscopy Fellowship and Hands-On Practice
Advanced endoscopy fellowships provide comprehensive training in both basic and complex procedures. Programs like the ASGE and JGES ESD Course, introduced in 2013, offer structured pathways for skill development14. These programs often include hands-on practice with animal models and supervised human cases14.
Case selection is critical during training. Larger lesions, such as those exceeding 20 mm, require more advanced skills and careful handling to minimize complications15. Mentorship plays a key role in guiding trainees through these challenging cases.
“Structured training programs are essential for advancing endoscopist competency and ensuring patient safety.”
Risks like hemorrhage, which occurs in 1.8% to 15.6% of cases, can be mitigated through proper technique and supervision14. Trainees at Brigham and Women’s Hospital completed an average of 72 ESDs, with 26 performed independently under supervision14.
- Training pathways emphasize hands-on practice and mentorship.
- Case selection is crucial for progressive skill development.
- Risks like perforation are higher in early training phases but can be reduced with structured programs.
- Fellowship opportunities provide comprehensive training in advanced techniques.
In conclusion, endoscopist training and skill development are foundational to achieving optimal procedural outcomes. Structured programs, mentorship, and careful case selection are essential components of this process.
Guidelines, Best Practices, and Future Research Directions
The evolution of endoscopic techniques has reshaped the approach to managing gastrointestinal lesions, with guidelines and research driving best practices. Published guidelines, such as those by the US Multi-Society Task Force and European associations, provide a foundation for clinical decision-making. These recommendations emphasize the importance of en bloc resection in reducing recurrence rates and improving long-term outcomes16.
Western Versus Eastern Perspectives
Regional practices in endoscopic techniques vary significantly between Western and Eastern centers. Western guidelines often prioritize mucosal resection for smaller lesions, while Eastern centers, particularly in Japan and South Korea, advocate for submucosal dissection even for larger lesions17. This divergence is rooted in differences in training, resource availability, and disease prevalence.
For instance, studies from Eastern centers report en bloc resection rates of 94.6% with submucosal dissection, compared to 44.5% in Western centers using mucosal resection16. These variations highlight the need for global collaboration to standardize best practices.
Emerging Trends and Research Priorities
Emerging trends in endoscopic techniques focus on device innovation and procedural refinement. Advances in imaging technologies, such as image-enhanced endoscopy, are improving lesion detection and characterization18. Additionally, research is exploring the cost-effectiveness of these techniques, particularly in low-resource settings.
Future priorities include long-term outcome analyses and collaborative studies to drive evidence-based improvements. For example, a recent study demonstrated that proficiency in submucosal dissection requires at least 47 procedures to achieve competency in en bloc resection16. Such findings underscore the importance of structured training programs.
“Global collaboration and standardized training are essential to advancing endoscopic techniques and improving patient outcomes.”
In conclusion, the integration of guidelines, regional practices, and emerging research is critical to optimizing endoscopic techniques. By addressing these factors, clinicians can enhance the management of gastrointestinal lesions and reduce recurrence rates.
Conclusion
The advancements in endoscopic techniques have significantly enhanced the precision and safety of lesion removal in gastroenterology. Both methods offer unique benefits, with one excelling in en bloc resection rates and the other in reduced procedure times19. Proper training and case selection remain critical to achieving optimal outcomes, particularly in complex cases involving the rectum.
Adherence to established guidelines ensures that clinicians can maximize the clinical benefit of these techniques. Recent studies highlight the importance of structured training programs, which reduce adverse events and improve procedural efficiency20. As the field continues to evolve, ongoing research and innovation will further refine these methods, enhancing patient safety and outcomes.
In conclusion, the choice of technique depends on lesion characteristics and center expertise. A tailored approach, guided by evidence-based practices, is essential for achieving successful removal and minimizing recurrence. The integration of advancements in the field will continue to shape the future of gastroenterology, offering improved benefits for patients worldwide.
FAQ
What is the difference between endoscopic mucosal resection and endoscopic submucosal dissection?
Which procedure has a lower recurrence rate for large colorectal polyps?
What are the primary risks associated with these procedures?
How does procedure time compare between EMR and ESD?
What training is required for performing ESD?
Are there specific guidelines for choosing between EMR and ESD?
What are the long-term benefits of ESD over EMR?
How do costs compare between EMR and ESD?
What are the key considerations for patient selection in these procedures?
What are the emerging trends in endoscopic resection techniques?
Source Links
- Underwater Techniques in Gastrointestinal Endoscopy: Diving into the Depths – https://www.mdpi.com/2072-6694/16/20/3535
- Endoscopic Mucosal Resection and Endoscopic Submucosal Dissection – https://pmc.ncbi.nlm.nih.gov/articles/PMC11309798/
- Endoscopic techniques for management of large colorectal polyps, strictures and leaks – https://pmc.ncbi.nlm.nih.gov/articles/PMC11296069/
- Approach Considerations, Endoscopic Mucosal Resection (EMR), Endoscopic Submucosal Dissection (ESD) – https://emedicine.medscape.com/article/1891659-technique
- Endoscopic resection of large non-pedunculated colorectal polyps: current standards of treatment – https://pmc.ncbi.nlm.nih.gov/articles/PMC11731078/
- Thieme E-Journals – Endoscopy / Full Text – https://www.thieme-connect.com/products/ejournals/html/10.1055/a-2304-3219
- Endoscopic Submucosal Dissection – https://my.clevelandclinic.org/podcasts/butts-and-guts/endoscopic-submucosal-dissection
- Learning curve for endoscopic submucosal dissection (ESD) in the United States: Large, untutored, single-operator experience – https://pmc.ncbi.nlm.nih.gov/articles/PMC11272410/
- PDF – https://gi.org/wp-content/uploads/2024/03/Lee_Mar2024_EBGI.pdf
- Endoscopic approach to large non-pedunculated colorectal polyps – https://pmc.ncbi.nlm.nih.gov/articles/PMC11842907/
- Clinical outcomes of colorectal neoplasm with positive resection margin after endoscopic submucosal dissection – Scientific Reports – https://www.nature.com/articles/s41598-024-63129-1
- ESD vs EMR for Large Non-Pedunculated Colon Polyps: Fewer Recurrences but More Complications – American College of Gastroenterology – https://gi.org/journals-publications/ebgi/lee_mar2024/
- Endoscopic Mucosal Resection (EMR) and Endoscopic Submucosal Dissection (ESD): Background, Indications, Contraindications – https://emedicine.medscape.com/article/1891659-overview
- Colorectal endoscopic submucosal dissection in the USA: The current state and future perspectives – https://pmc.ncbi.nlm.nih.gov/articles/PMC11194299/
- Large nonpedunculated colorectal polyp management through the lens of an interventional endoscopist – https://www.canjsurg.ca/content/67/5/E345
- Advanced endoscopic resection for early gastrointestinal cancers in India: Challenges and opportunities await! – Indian Journal of Gastroenterology – https://link.springer.com/article/10.1007/s12664-024-01686-z
- Post-polypectomy colorectal bleeding: current strategies and the way forward – https://www.e-ce.org/journal/view.php?number=7956
- A novel nomogram for the prediction of perforation during endoscopic submucosal dissection for colorectal neoplasms – https://pmc.ncbi.nlm.nih.gov/articles/PMC11379254/
- Endoscopic resection of large non-pedunculated colorectal polyps: current standards of treatment – https://egastroenterology.bmj.com/content/2/2/e100025
- Underwater endoscopic mucosal resection is superior to conventional endoscopic mucosal resection for medium-sized colorectal sessile polyps: a randomized controlled trial – Scientific Reports – https://www.nature.com/articles/s41598-024-81817-w