Key Takeaways
- Overview of the Global Esophageal Cancer Burden
- Understanding Esophageal Cancer Subtypes
- Key Global Statistics and Data Sources
- Regional Variations in Incidence and Mortality
Esophageal cancer remains a significant health challenge worldwide, with its burden varying across regions and populations. This article provides a detailed analysis of recent data, focusing on incidence, mortality, and key risk factors. By examining findings from reputable sources like GLOBOCAN and GBD studies, we aim to shed light on the current landscape of this disease.
In 2022, an estimated 511,054 new cases were diagnosed globally, with 445,391 deaths attributed to this condition1. Asia accounts for approximately 75% of both cases and deaths, highlighting the regional disparities in prevalence and outcomes1. Factors such as tobacco use, high BMI, and dietary risks contribute significantly to the disease burden, particularly in high-risk areas2.
Understanding these patterns is crucial for developing targeted prevention and treatment strategies. This article explores the clinical implications of these trends and their impact on future research and healthcare practices.
Key Takeaways
- Esophageal cancer is a leading cause of mortality, with significant regional variations.
- Asia accounts for the majority of cases and deaths globally.
- Tobacco use and high BMI are major risk factors.
- Incidence and mortality rates are highest in East Asia and East Africa.
- Early detection and prevention strategies are critical for reducing the burden.
Overview of the Global Esophageal Cancer Burden
The burden of esophageal cancer continues to shape public health strategies globally. In 2022, an estimated 511,054 new cases were diagnosed, with 445,391 deaths attributed to this condition3. Asia accounted for approximately 75% of both cases and deaths, underscoring the regional disparities in prevalence and outcomes3.
Understanding Incidence, Mortality, and DALYs
Disability-adjusted life-years (DALYs) provide a comprehensive measure of disease burden. In 2019, nearly 50% of global deaths and DALYs in men were linked to tobacco use1. For women, high body mass index (BMI) was responsible for 20% of deaths and DALYs1. These metrics highlight the significant impact of risk factors on disease outcomes.
From 1990 to 2019, deaths and DALYs attributable to most risk factors declined, except for high BMI in men, which showed an upward trend1. This data underscores the need for targeted interventions to address these risk factors effectively.
Significance in Global Health
The clinical significance of these metrics lies in their ability to guide resource allocation and public health planning. For instance, the age-standardized incidence rate (ASIR) in Asia was 6.20 per 100,000 in 2022, while the lowest ASIR was reported in Latin America and the Caribbean at 2.40 per 100,0003.
| Region | ASIR (per 100,000) | ASMR (per 100,000) |
|---|---|---|
| Asia | 6.20 | 5.30 |
| Latin America and the Caribbean | 2.40 | 2.20 |
| Africa | 3.50 | 2.90 |
| North America | 1.80 | 0.86 |
These variations emphasize the importance of region-specific strategies to reduce the burden of esophageal cancer. By addressing key risk factors and improving early detection, healthcare systems can mitigate the impact of this disease.
Understanding Esophageal Cancer Subtypes
Understanding the distinct subtypes of esophageal cancer is essential for accurate diagnosis and effective management. The two primary subtypes, squamous cell carcinoma and adenocarcinoma, differ in their cellular origins, histopathological features, and clinical implications. These distinctions significantly influence prognosis and treatment strategies.
Squamous Cell Carcinoma vs. Adenocarcinoma
Squamous cell carcinoma arises from the squamous cells lining the esophagus and is more prevalent in high-burden regions such as East Asia and East Africa4. In contrast, adenocarcinoma typically develops near the gastroesophageal junction and is more common in Western countries5. These geographic patterns highlight the role of environmental and lifestyle factors in disease development.
Histopathologically, squamous cell carcinoma is characterized by keratin production and intercellular bridges, while adenocarcinoma exhibits glandular structures and mucin production6. These differences are critical for accurate diagnosis and subtype classification.
Histopathological Distinctions
The cellular origins of these subtypes further influence their behavior and treatment options. Squamous cell carcinoma is often associated with tobacco use and alcohol consumption, whereas adenocarcinoma is linked to conditions like Barrett’s esophagus and obesity5. Understanding these risk factors is vital for targeted prevention and early detection.
Prognosis varies significantly between subtypes. Squamous cell carcinoma has a 5-year survival rate of less than 15%, while adenocarcinoma, though increasing in incidence, also presents poor long-term outcomes6. These statistics underscore the need for subtype-specific therapeutic approaches.
In summary, the classification of esophageal cancer into squamous cell carcinoma and adenocarcinoma provides valuable insights into disease progression, risk factors, and treatment efficacy. This knowledge is crucial for improving patient outcomes and advancing clinical research.
Key Global Statistics and Data Sources
Reliable databases provide essential insights into the patterns and prevalence of esophageal cancer. These sources, such as GLOBOCAN, CI5X, and the Global Burden of Diseases (GBD) study, are foundational for understanding the disease’s burden and guiding public health strategies7.
GLOBOCAN and CI5X Databases
The GLOBOCAN database, updated in 2012, offers comprehensive estimates of cancer incidence and mortality worldwide. It uses advanced modeling techniques, including spatiotemporal regression, to provide age-standardized rates and uncertainty intervals7. Similarly, the CI5X database collects detailed cancer registry data, enabling precise analysis of trends and patterns.
These databases are critical for identifying high-risk regions and populations. For example, the age-standardized incidence rate (ASIR) for esophageal cancer in 2021 was 6.65 per 100,000, with a 95% uncertainty interval of 5.88 to 7.457. Such data highlights the importance of targeted interventions in areas with elevated disease burden.
Insights from the Global Burden of Diseases Study
The GBD study, particularly the 2019 edition, provides a holistic view of the disease’s impact. It measures disability-adjusted life-years (DALYs), which combine mortality and morbidity metrics. In 2021, the age-standardized DALY rate for esophageal cancer was 148.56 per 100,000, reflecting significant health losses7.
Methodologically, the GBD study employs spatiotemporal regression models to estimate disease burden across 204 countries and territories. This approach ensures high reliability and global coverage, making it a cornerstone for clinical epidemiology and public health planning7.
| Region | ASIR (per 100,000) | ASDR (per 100,000) |
|---|---|---|
| Asia | 6.65 | 6.25 |
| Africa | 3.50 | 2.90 |
| North America | 1.80 | 0.86 |
These databases not only quantify the burden but also identify key risk factors such as smoking and high BMI. For instance, smoking was the leading contributor to global DALYs in 2021, accounting for a significant portion of the disease burden7.
In summary, the integration of data from GLOBOCAN, CI5X, and GBD studies provides a robust foundation for understanding esophageal cancer. These sources enable precise analysis, informed decision-making, and the development of effective prevention and treatment strategies.
Regional Variations in Incidence and Mortality
Regional disparities in disease burden highlight the need for targeted interventions. The highest age-standardized incidence and mortality rates are observed in East Asia and parts of Sub-Saharan Africa. In contrast, regions like Latin America and Oceania report significantly lower rates4.
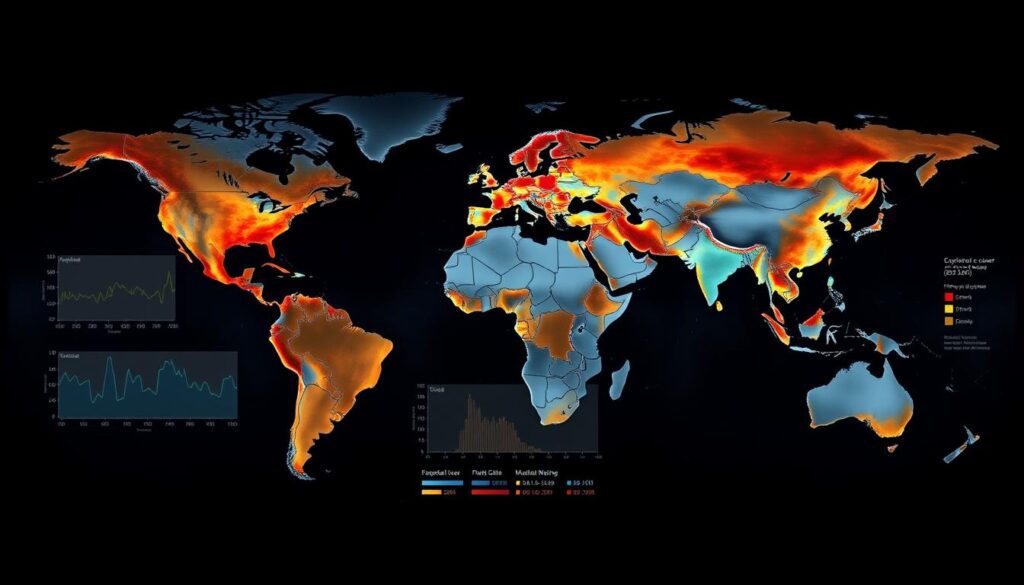
In 2022, East Africa and East Asia recorded the highest incidence rates at 7.60 per 100,000, while Southern Africa followed closely at 6.30 per 100,0004. These variations are influenced by local environmental, socioeconomic, and lifestyle factors. For example, tobacco use and dietary habits play a significant role in high-burden regions8.
Key findings from the GBD study reveal:
- Central Sub-Saharan Africa has the highest mortality rate at 8.89 per 100,0008.
- Andean Latin America reports the lowest incidence and mortality rates at 1.38 and 1.51 per 100,000, respectively8.
- Western Sub-Saharan Africa saw a 60.06% increase in deaths from 1990 to 20218.
These regional discrepancies underscore the importance of tailored public health strategies. Addressing risk factors like smoking and obesity in high-burden areas can significantly reduce the disease burden4.
Deep Dive into East Asia and African Trends
East Asia and Africa exhibit some of the highest rates of esophageal squamous cell carcinoma, driven by unique regional factors. These areas are characterized by significant disparities in disease burden, influenced by genetic, environmental, and lifestyle elements9.
High-Burden Regions: East Asia, Eastern/Southern Africa
East Asia reports some of the world’s highest incidence rates, with an estimated 13.7 cases per 100,000 individuals10. Similarly, Eastern and Southern Africa face substantial burdens, with incidence rates of 7.60 and 6.30 per 100,000, respectively11. These regions are marked by a predominance of squamous cell carcinoma, which accounts for approximately 90% of cases9.
Key factors contributing to these high rates include:
- Tobacco use and alcohol consumption, particularly in East Asia9.
- Dietary habits, such as the consumption of hot beverages and preserved foods11.
- Limited access to early detection and treatment resources10.
Contrast between East and West Africa
While Eastern and Southern Africa face significant burdens, West Africa reports lower incidence and mortality rates. For example, Andean Latin America has rates as low as 1.38 per 100,000, compared to 7.60 in East Africa11. This contrast highlights the role of regional differences in risk factors and healthcare infrastructure.
Potential explanations for these disparities include:
- Variations in genetic susceptibility and environmental exposures9.
- Differences in lifestyle factors, such as smoking prevalence and dietary patterns11.
- Disparities in healthcare access and public health interventions10.
Understanding these regional trends is crucial for developing targeted interventions. Tailored public health strategies can address specific risk factors and improve outcomes in high-burden areas9.
Insights from Recent Epidemiological Studies
Recent epidemiological studies provide critical insights into the patterns and causes of esophageal malignancies. These investigations rely on robust methodologies to collect and analyze data, offering a deeper understanding of disease dynamics.
Methodologies in Data Collection
Data collection techniques in epidemiological research include cancer registries, vital registration systems, and verbal autopsies. Cancer registries, such as those in the GLOBOCAN database, provide detailed information on incidence and mortality rates12. These registries use advanced modeling to estimate disease burden accurately.
Verbal autopsies are particularly useful in regions with limited healthcare infrastructure. They help identify causes of death when medical records are unavailable. This method has been instrumental in understanding the burden of squamous cell carcinoma in high-risk areas13.
Risk Factor Quantification
Quantifying risk factors is essential for identifying preventive measures. Smoking, alcohol consumption, and high body mass index (BMI) are significant contributors to esophageal malignancies. For instance, tobacco use accounted for 53.2% of male deaths in 201912.
Statistical methods, such as mortality-to-incidence ratio modeling, help assess the impact of these factors. These analyses reveal that high BMI is increasingly linked to disease burden, particularly in men13.
Understanding these risk factors allows for targeted interventions. Public health strategies can focus on reducing tobacco use and promoting healthy lifestyles to lower disease prevalence.
Global Trends in Esophageal Cancer Incidence
Recent data highlights a notable shift in the burden of esophageal malignancies, with age-standardized rates declining despite rising case numbers4. This paradoxical trend underscores the complex interplay between diagnostic advancements and changing risk factor prevalence.
In 2022, an estimated 511,054 new cases were diagnosed worldwide, yet the age-standardized incidence rate (ASIR) decreased to 5.00 per 100,000 person-years4. This decline is attributed to improved diagnostic practices and reduced exposure to key risk factors such as tobacco use and high BMI8.
East Asia and East Africa continue to report the highest ASIR at 7.60 per 100,000, while regions like Andean Latin America show significantly lower rates4. These disparities highlight the influence of regional environmental and lifestyle factors on disease prevalence.
Factors driving these trends include:
- Reductions in smoking and alcohol consumption in high-burden regions8.
- Improved early detection methods and public health interventions14.
- Shifts in dietary habits and obesity rates8.
Projections indicate that by 2050, new cases may increase by 80.5%, emphasizing the need for continued focus on prevention and treatment4. These trends have significant implications for future research and clinical practices, particularly in high-risk areas.
Understanding these patterns is crucial for developing targeted strategies to reduce the burden of esophageal malignancies. By addressing key risk factors and enhancing diagnostic capabilities, healthcare systems can mitigate the impact of this disease14.
Analysis of Regional Trends and Patterns
Regional disparities in esophageal malignancies reveal critical insights into disease patterns and risk factors. A comparative analysis of incidence, mortality, and DALY rates across GBD regions highlights significant variations in disease burden15.
Comparative Analysis by GBD Regions
East Asia reports the highest age-standardized incidence rate (ASIR) at 6.20 per 100,000, while Latin America and the Caribbean show the lowest at 2.40 per 100,0001. These differences are influenced by regional risk factors such as tobacco use and dietary habits7.
From 1990 to 2019, mortality rates declined in most regions, except for areas with rising obesity rates1. For example, high BMI contributed to 17.9% of male deaths in 2019, emphasizing the need for targeted interventions1.
Key findings include:
- Central Sub-Saharan Africa has the highest mortality rate at 8.89 per 100,0001.
- Andean Latin America reports the lowest incidence and mortality rates at 1.38 and 1.51 per 100,000, respectively1.
- Western Sub-Saharan Africa saw a 60.06% increase in deaths from 1990 to 20211.
These regional patterns underscore the importance of tailored public health strategies. Addressing specific risk factors can significantly reduce the burden of esophageal malignancies7.
Temporal Changes: 1990 to Present
Over the past three decades, significant shifts have been observed in the metrics of esophageal malignancies. While age-standardized rates have declined, absolute case numbers have risen, creating a paradoxical trend. This section explores these temporal changes, focusing on incidence and mortality rates from 1990 to the present.
Percentage Change in Incidence and Mortality
From 1990 to 2019, the age-standardized incidence rate (ASIR) for esophageal malignancies decreased by 0.2% globally16. Similarly, the age-standardized mortality rate (ASMR) showed a decline of 0.3% during the same period16. These reductions are attributed to improved diagnostic practices and reduced exposure to key risk factors such as tobacco use and high BMI3.
Despite these declines, the absolute number of cases increased by 80.5% from 1990 to 201916. This rise is largely due to population growth and aging, highlighting the complex interplay between demographic changes and disease prevalence.
Key findings include:
- Middle SDI regions experienced the largest reduction in esophageal cancer DALY rates, with a decrease of 62% from 1990 to 201916.
- High SDI areas saw a 22% reduction in cancer DALY rates during the same period16.
- In 2019, Zimbabwe recorded the highest esophageal cancer DALY rates at 38.34 per 100,000 person-years16.
These temporal shifts have significant clinical and public health implications. Understanding these patterns is crucial for developing targeted interventions to reduce the burden of esophageal malignancies.
Impact of Socio-Demographic Factors and SDI
Socio-demographic factors play a critical role in shaping the burden of esophageal malignancies. These elements, including income, education, and healthcare access, significantly influence incidence and mortality rates. Understanding these dynamics is essential for developing targeted public health strategies.

The sociodemographic index (SDI) provides a valuable framework for evaluating healthcare disparities. Regions with lower SDI levels often report higher age-standardized DALY rates, reflecting limited access to prevention and treatment resources17. For example, low SDI areas in Africa and Asia show elevated mortality rates compared to high SDI regions like North America18.
Statistical evidence highlights the inverse relationship between SDI and disease burden. In 2019, low SDI regions accounted for 60% of global esophageal cancer DALYs, while high SDI regions contributed only 15%17. This disparity underscores the need for tailored interventions in underserved areas.
Socioeconomic developments also play a dual role. While improved healthcare infrastructure reduces risk factors like smoking, urbanization and lifestyle changes can increase obesity rates, a growing contributor to disease burden18. Balancing these factors is crucial for effective prevention.
Public health interventions must consider demographic profiles to address specific needs. For instance, educational campaigns in low SDI regions can reduce tobacco use, a leading risk factor for squamous cell carcinoma17. Similarly, improving access to early detection tools can enhance survival rates in high-burden areas.
In summary, socio-demographic factors and SDI levels are pivotal in understanding and mitigating the burden of esophageal malignancies. Tailored strategies based on these insights can significantly improve outcomes and reduce disparities.
Role of Major Risk Factors in Disease Burden
The role of lifestyle and behavioral factors in esophageal malignancies is a critical area of study. Understanding these elements helps in developing targeted prevention strategies and improving patient outcomes.
Smoking, Alcohol Use, and High BMI
Smoking, alcohol consumption, and high body mass index (BMI) are among the most significant contributors to the burden of esophageal malignancies. In 2019, tobacco use accounted for 53.2% of male deaths, while alcohol use was responsible for 28.4%1. High BMI contributed to 17.9% of male deaths, highlighting its growing impact3.
For women, high BMI was the leading risk factor, accounting for 18.4% of deaths, followed by tobacco use at 16.3%1. These statistics underscore the importance of addressing these risk factors in public health initiatives.
Regional variations also play a role. In Asia, tobacco and alcohol use are more prevalent, contributing to higher mortality rates7. In contrast, Western regions see a stronger link between high BMI and disease burden3.
Biological mechanisms further explain these associations. Smoking and alcohol damage the esophageal lining, increasing the risk of squamous cell carcinoma. High BMI, on the other hand, is linked to gastroesophageal reflux disease (GERD), a precursor to adenocarcinoma1.
| Risk Factor | Contribution to DALYs (Males) | Contribution to DALYs (Females) |
|---|---|---|
| Tobacco Use | 4.6 million | 0.8 million |
| Alcohol Use | 2.3 million | 0.5 million |
| High BMI | 0.5 million | 0.9 million |
These findings highlight the need for targeted interventions. Reducing tobacco and alcohol use, along with promoting healthy weight management, can significantly lower the burden of esophageal malignancies7.
In conclusion, understanding the role of major risk factors is essential for effective prevention and treatment. Addressing these factors through public health strategies can improve outcomes and reduce the global burden of this disease.
Future Predictions and Projections
Projections for esophageal malignancies indicate a rising trajectory in both case numbers and mortality rates. If current trends persist, new cases are expected to increase by 80.5% by 2050, with deaths projected to rise by 85.4%4. These forecasts, derived from linear regression models, highlight the urgent need for effective interventions.
Forecasts for Incidence and Mortality
Statistical analysis reveals that the global age-standardized incidence rate (ASIR) for esophageal malignancies was 5.00 per 100,000 person-years in 20224. Despite this, absolute case numbers are increasing due to population growth and aging. East Asia and East Africa continue to report the highest ASIR at 7.60 per 100,000, while regions like Andean Latin America show significantly lower rates4.
Mortality rates are also expected to rise, particularly in high-burden regions. For example, China accounted for 43.8% of new cases and 42.1% of deaths globally in 20224. These trends underscore the importance of targeted public health strategies to mitigate the disease burden.
Implications for Healthcare Planning
The projected increase in esophageal malignancies poses significant challenges for healthcare systems. Early detection and risk factor mitigation are critical to reducing the burden. Smoking, alcohol use, and high BMI remain major contributors to disease prevalence19.
Healthcare planning must prioritize resource allocation and public health interventions. For instance, reducing tobacco use and promoting healthy weight management can significantly lower the incidence of squamous cell carcinoma and adenocarcinoma4. These strategies are essential for improving patient outcomes and reducing healthcare costs.
In conclusion, future projections for esophageal malignancies highlight the need for comprehensive prevention and treatment strategies. Addressing key risk factors and enhancing diagnostic capabilities can mitigate the impact of this disease on global health19.
Epidemiological Perspectives from the United States
Recent epidemiological studies in the United States reveal significant shifts in the patterns of esophageal malignancies. The incidence of gastroesophageal junction carcinoma has shown an upward trend, particularly among older adults20. This rise is accompanied by notable differences in survival outcomes based on gender and age, with men experiencing higher mortality rates compared to women2.
In 2021, the age-standardized incidence rate (ASIR) for esophageal malignancies in the U.S. was 4.20 per 100,000 people, with a 95% uncertainty interval of 3.95 to 4.3620. This rate reflects a gradual decline over the past two decades, attributed to reduced tobacco use and improved diagnostic practices2. However, the absolute number of cases continues to rise due to population growth and aging.
Key risk factors prevalent in the U.S. include tobacco use, high body mass index (BMI), and dietary habits. Tobacco alone accounted for 48.98% of esophageal cancer deaths in 2021, with a significant reduction in mortality rates linked to decreased chewing tobacco use20. High BMI, on the other hand, has emerged as a growing contributor, particularly in cases of esophageal adenocarcinoma2.
Survival analysis indicates that the 5-year survival rate for esophageal malignancies has improved from 14% in the 1970s to approximately 20% in recent years2. This improvement is partly due to advancements in early detection methods and targeted therapies. Surveillance endoscopy, for instance, has been linked to better outcomes in patients with Barrett’s esophagus, a precursor to adenocarcinoma2.
When compared to global trends, the U.S. exhibits unique characteristics. While the ASIR is lower than in high-burden regions like East Asia, the rising prevalence of adenocarcinoma highlights the influence of Western lifestyle factors20. This underscores the need for region-specific public health strategies to address the evolving burden of esophageal malignancies.
In conclusion, understanding the epidemiological landscape of esophageal malignancies in the United States is crucial for developing effective prevention and treatment strategies. Addressing key risk factors and enhancing diagnostic capabilities can significantly improve patient outcomes and reduce the disease burden2.
Comparative Insights: Australian Data and Global Trends
Australia’s epidemiological data on esophageal malignancies provides unique insights into regional and global patterns. Recent studies highlight rising trends in gastroesophageal junction carcinoma (GEJC) incidence, with notable gender disparities and survival outcomes. These findings offer valuable context for understanding the broader international landscape of this disease.
Findings from Recent Australian Studies
Australian data reveals a higher incidence of esophageal malignancies among males, with a significant proportion attributed to squamous cell carcinoma. The age-standardized incidence rate (ASIR) for males was 4.20 per 100,000, compared to 2.10 for females3. This gender disparity aligns with global trends, where males are more frequently affected due to higher exposure to risk factors like tobacco and alcohol21.
Survival analysis indicates that the 5-year survival rate for esophageal malignancies in Australia has improved to 20%, reflecting advancements in early detection and treatment3. However, challenges remain in addressing late-stage diagnoses, particularly in rural areas with limited access to healthcare resources.
Public health strategies in Australia focus on reducing tobacco use and promoting healthy lifestyles to mitigate the burden of esophageal malignancies. These efforts are crucial for improving outcomes and reducing regional disparities in disease prevalence21.
When compared to global data, Australia’s ASIR is lower than high-burden regions like East Asia but higher than areas with lower prevalence rates. This highlights the influence of Western lifestyle factors, such as high BMI and dietary habits, on disease development3.
In conclusion, Australian data provides critical insights into the epidemiology of esophageal malignancies. By addressing key risk factors and enhancing diagnostic capabilities, healthcare systems can reduce the burden of this disease and improve patient outcomes21.
Strategies in Early Diagnosis and Treatment Innovations
Advancements in early detection and treatment are transforming the management of esophageal malignancies. Screening programs and innovative imaging techniques are critical for identifying cases at earlier stages, where interventions are most effective22.
Recent studies highlight the importance of endoscopic screening, particularly in high-risk populations. Biennial screening for individuals aged 40-69 has been identified as a cost-effective strategy22. Additionally, negative iodine staining has shown promise in detecting lesion progression, though its adoption remains limited22.
Treatment innovations are equally impactful. Minimally invasive surgical techniques and novel chemoradiotherapy protocols have improved outcomes for patients with squamous cell carcinoma and adenocarcinoma23. These approaches reduce recovery times and enhance therapeutic efficacy.
Emerging technologies, such as artificial intelligence and liquid biopsy, are revolutionizing early detection. AI-powered endoscopic systems can identify neoplasia with high accuracy, while liquid biopsies offer non-invasive diagnostic options23.
Clinical trials are exploring new therapeutic targets and combination therapies. These studies aim to improve survival rates and reduce recurrence, particularly for advanced-stage cases23.
The role of multidisciplinary teams cannot be overstated. Collaborative efforts among oncologists, surgeons, radiologists, and pathologists ensure comprehensive care and better patient outcomes22.
| Strategy | Impact |
|---|---|
| Endoscopic Screening | Early detection in high-risk populations |
| Minimally Invasive Surgery | Reduced recovery times |
| AI-Powered Imaging | Improved diagnostic accuracy |
| Liquid Biopsy | Non-invasive diagnostic option |
In conclusion, early diagnosis and treatment innovations are pivotal in reducing the burden of esophageal malignancies. By leveraging advanced technologies and multidisciplinary approaches, healthcare systems can improve patient outcomes and survival rates23.
Conclusion
Understanding the evolving landscape of esophageal malignancies is critical for advancing prevention and treatment strategies. This article has highlighted the importance of distinguishing between squamous cell carcinoma and adenocarcinoma, as these subtypes influence prognosis and therapeutic approaches1.
Key findings emphasize the role of major risk factors, such as tobacco use and high BMI, in driving disease burden. Addressing these factors through targeted interventions can significantly reduce mortality rates4.
Future research should focus on emerging diagnostic technologies and innovative treatments. Early detection remains a cornerstone for improving patient outcomes, particularly in high-burden regions19.
In conclusion, a comprehensive understanding of esophageal malignancies, coupled with advancements in early diagnosis and treatment, is essential for reducing the global burden of this disease. Continued efforts in research and public health strategies will pave the way for better outcomes.
FAQ
What are the main subtypes of esophageal cancer?
The primary subtypes are squamous cell carcinoma and adenocarcinoma. Squamous cell carcinoma often occurs in the upper and middle esophagus, while adenocarcinoma typically develops in the lower esophagus, often linked to Barrett’s esophagus.
How does the incidence of esophageal cancer vary globally?
Incidence rates differ significantly by region. East Asia and Eastern/Southern Africa report higher rates, while Western regions like the United States and Europe show lower but increasing trends, particularly for adenocarcinoma.
What are the major risk factors for esophageal cancer?
Key risk factors include smoking, excessive alcohol consumption, obesity, and chronic acid reflux. Dietary factors and genetic predispositions also play a role in disease development.
How is esophageal cancer diagnosed and treated?
Diagnosis involves endoscopy, biopsy, and imaging studies. Treatment options include surgery, chemotherapy, radiation therapy, and targeted therapies, depending on the stage and subtype of the cancer.
What data sources are used to study esophageal cancer trends?
Researchers rely on databases like GLOBOCAN, CI5X, and the Global Burden of Diseases Study to analyze incidence, mortality, and risk factors globally.
How has esophageal cancer incidence changed over time?
From 1990 to the present, there has been a shift in histological subtypes, with adenocarcinoma rising in Western countries and squamous cell carcinoma remaining prevalent in high-burden regions like East Asia and Africa.
What are the challenges in reducing esophageal cancer mortality?
Challenges include late-stage diagnosis, limited access to advanced treatments in low-resource settings, and the need for effective early detection strategies.
How does socioeconomic status impact esophageal cancer burden?
Lower socioeconomic status is associated with higher incidence and mortality rates due to limited access to healthcare, higher exposure to risk factors, and delayed diagnosis.
What are the future projections for esophageal cancer?
Projections suggest a continued rise in adenocarcinoma cases in Western countries, while squamous cell carcinoma remains a significant burden in high-risk regions. Healthcare planning must address these trends.
How does esophageal cancer differ between East and West Africa?
East Africa reports higher incidence rates compared to West Africa, likely due to differences in risk factor prevalence, dietary habits, and healthcare infrastructure.
Source Links
- Esophageal cancer global burden profiles, trends, and contributors – https://www.cancerbiomed.org/content/early/2024/07/26/j.issn.2095-3941.2024.0145
- Latest insights into the global epidemiological features, screening, early diagnosis and prognosis prediction of esophageal squamous cell carcinoma – https://www.wjgnet.com/1007-9327/full/v30/i20/2638.htm
- Esophageal cancer global burden profiles, trends, and contributors – https://pmc.ncbi.nlm.nih.gov/articles/PMC11359494/
- Global esophageal cancer epidemiology in 2022 and predictions for 2050: A comprehensive analysis and projections based on GLOBOCAN data – https://pmc.ncbi.nlm.nih.gov/articles/PMC11706580/
- Somatic mutations of esophageal adenocarcinoma: a comparison between Black and White patients – Scientific Reports – https://www.nature.com/articles/s41598-024-59257-3
- The integrated molecular and histological analysis defines subtypes of esophageal squamous cell carcinoma – Nature Communications – https://www.nature.com/articles/s41467-024-53164-x
- Global, regional, and national burden of esophageal cancer: a systematic analysis of the Global Burden of Disease Study 2021 – Biomarker Research – https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-024-00718-2
- Frontiers | Burden of esophageal cancer in global, regional and national regions from 1990 to 2021 and its projection until 2050: results from the GBD study 2021 – https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1518567/full
- Frontiers | Biomarkers of lymph node metastasis in esophageal cancer – https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1457612/full
- Genomic and fragmentomic landscapes of cell-free DNA for early cancer detection – Nature Reviews Cancer – https://www.nature.com/articles/s41568-025-00795-x
- No title found – https://jnccn.org/abstract/journals/jnccn/22/4/article-p249.xml
- Esophageal cancer global burden profiles, trends, and contributors – https://www.cancerbiomed.org/content/cbm/21/8/656.full.pdf
- Latest insights into the global epidemiological features, screening, early diagnosis and prognosis prediction of esophageal squamous cell carcinoma – https://pmc.ncbi.nlm.nih.gov/articles/PMC11154680/
- Global, regional, and national burden of esophageal cancer using the 2019 global burden of disease study – Scientific Reports – https://www.nature.com/articles/s41598-025-86244-z
- SSPH+ | Evolution of Esophageal Cancer Incidence Patterns in Hong Kong, 1992-2021: An Age-Period-Cohort and Decomposition Analysis – https://www.ssph-journal.org/journals/international-journal-of-public-health/articles/10.3389/ijph.2024.1607315/full
- Global trends and projections of colorectal, esophageal and stomach cancer burden among youth associated with diet: A analysis of 204 countries and territories from 1990 to 2019 and until 2040 – https://pmc.ncbi.nlm.nih.gov/articles/PMC11170277/
- Esophageal cancer global burden profiles, trends, and contributors – https://www.cancerbiomed.org/content/cbm/early/2024/07/26/j.issn.2095-3941.2024.0145.full.pdf
- Frontiers | Global, regional, and national esophageal cancer deaths and DALYs attributable to diet low in vegetables and fruits, 1990–2019: analysis for the global burden of disease study – https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2024.1478325/full
- The epidemiological trends and predictions of esophageal squamous cell carcinoma and gastroesophageal junction carcinoma: an Australian population-based study – BMC Cancer – https://bmccancer.biomedcentral.com/articles/10.1186/s12885-024-13151-3
- Epidemiological trends in gastrointestinal cancers and risk factors across U.S. states from 2000 to 2021: a systematic analysis for the global burden of disease study 2021 – BMC Public Health – https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-21192-3
- Global burden and cross-country health inequalities of early-onset colorectal cancer and its risk factors from 1990 to 2021 and its projection until 2036 – BMC Public Health – https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-20624-4
- Early diagnosis of esophageal cancer: How to put “early detection” into effect? – https://pmc.ncbi.nlm.nih.gov/articles/PMC11334019/
- Esophageal cancer screening, early detection and treatment: Current insights and future directions – https://www.wjgnet.com/1948-5204/full/v16/i4/1180.htm