Key Takeaways
- Understanding IBD and Colorectal Cancer Risks
- Historical Evolution of Colonoscopy in IBD Surveillance
- Current Guidelines for IBD Colonoscopic Surveillance
- High Definition White Light Endoscopy in IBD
Inflammatory bowel disease (IBD) patients face a heightened risk of colorectal cancer (CRC), making precise monitoring essential. Advanced imaging technologies, such as high-definition scopes and chromoendoscopy, have significantly improved the detection of dysplastic lesions in individuals with ulcerative colitis and Crohn’s disease1.
These innovations allow for better visualization of the colonic mucosa, enabling earlier identification of abnormalities. Targeted biopsies, combined with advanced imaging, have become a cornerstone in managing colitis-related dysplasia2. This approach ensures that potential risks are addressed promptly, reducing the likelihood of progression to CRC.
Recent guidelines emphasize the importance of precision in surveillance protocols. High-definition endoscopy and targeted sampling methods are now recommended to enhance diagnostic accuracy3. This article explores the evolution of these techniques, current best practices, and their role in improving outcomes for IBD patients.
Key Takeaways
- Advanced imaging improves dysplasia detection in IBD patients.
- High-definition scopes enhance mucosal visualization.
- Targeted biopsies are critical for accurate diagnosis.
- Precision in surveillance reduces CRC risk.
- Current guidelines support the use of advanced endoscopic techniques.
Understanding IBD and Colorectal Cancer Risks
Chronic inflammation in the bowel significantly elevates the risk of colorectal cancer, particularly in patients with inflammatory bowel disease. This connection is driven by prolonged exposure to inflammatory processes, which can lead to cellular damage and genomic instability4.
Overview of Inflammatory Bowel Disease
Inflammatory bowel disease encompasses conditions like ulcerative colitis and Crohn’s disease, both characterized by chronic inflammation of the gastrointestinal tract. These conditions disrupt normal tissue repair mechanisms, increasing intestinal permeability and allowing harmful luminal factors to penetrate4.
Recent studies highlight that the global incidence of IBD is rising, making it crucial to understand its link to colorectal neoplasia4. Early diagnosis of these conditions is vital, as it enables timely surveillance and reduces the likelihood of missed dysplasia.
Identifying Colorectal Cancer Risk Factors
Several factors contribute to the heightened risk of colorectal cancer in IBD patients. Family history, disease severity, and the duration of inflammation are critical determinants4. Prolonged inflammation, especially when combined with immunosuppressive therapies, further escalates cancer risk4.
Key inflammatory pathways, such as IL-6/STAT3 and NF-κB, are activated in colitis-associated colorectal cancer, promoting cell survival and resistance to apoptosis4. Additionally, genomic instability, indicated by chromosomal abnormalities, plays a pivotal role in the early stages of cancer development4.
Surveillance strategies, including advanced diagnostic imaging, are essential for early detection. Studies show that interval cancer rates in IBD patients can reach up to 32%, underscoring the need for improved monitoring techniques4.
Historical Evolution of Colonoscopy in IBD Surveillance
The approach to monitoring patients with chronic bowel conditions has evolved significantly over the decades. Early methods relied heavily on random biopsy techniques, which involved taking tissue samples from multiple areas of the colon without specific targeting. This approach was based on the assumption that dysplasia, a precursor to cancer, could be evenly distributed throughout the bowel5.
However, random biopsy protocols had notable limitations. Studies revealed that these methods often missed invisible dysplasia, leading to delayed diagnoses. The detection rates for abnormal tissue were inconsistent, and the process was time-consuming and resource-intensive6. These challenges highlighted the need for more precise monitoring strategies.
Advancements in endoscopic imaging marked a turning point in bowel monitoring. The introduction of high-definition scopes and chromoendoscopy allowed for better visualization of the colonic mucosa. Dye-based techniques enhanced the contrast between normal and abnormal tissue, making it easier to identify suspicious areas7. This shift toward targeted biopsy methods significantly improved dysplasia detection rates.
Clinical evidence played a crucial role in this transition. Research demonstrated that targeted biopsy approaches, combined with advanced imaging, were more effective than random sampling. Technological updates, such as the integration of digital imaging systems, further refined the precision of these techniques5. Today, these advancements are widely adopted in clinical practice, reflecting the ongoing commitment to improving patient outcomes.
- Random biopsy techniques were the standard before high-definition imaging.
- Early methods often missed invisible dysplasia, leading to delayed diagnoses.
- Chromoendoscopy and targeted biopsies improved detection rates significantly.
- Technological updates and clinical evidence shaped current practices.
Current Guidelines for IBD Colonoscopic Surveillance
International guidelines have refined strategies for monitoring patients with chronic bowel conditions. These protocols emphasize precision in identifying dysplasia and reducing cancer risk through standardized practices8.
Key Recommendations from International Societies
The 2015 SCENIC guidelines, along with subsequent updates, advocate for the use of high-definition and dye-based techniques as the standard of care. These methods enhance the detection of visible and invisible dysplasia, improving diagnostic accuracy9.
Surveillance intervals vary based on individual risk factors. For example, patients with ulcerative colitis should begin screening 8 years after symptom onset, with follow-ups every 1-3 years. Those with primary sclerosing cholangitis require annual monitoring8.
Risk stratification is critical in determining the frequency of surveillance colonoscopy. High-risk patients, such as those with a family history of colorectal cancer or severe inflammation, may need more frequent evaluations9.
Definitions and Management of Dysplasia
Guidelines provide clear definitions for visible and invisible dysplasia. Visible lesions are identified during endoscopy, while invisible dysplasia is detected through biopsy. Management depends on resectability and complete endoscopic removal8.
For resectable dysplasia, endoscopic removal is recommended, followed by close monitoring. Non-resectable cases may require surgical intervention. These strategies aim to reduce progression to colorectal cancer9.
Evolving Practice Guidelines
Recent literature highlights the importance of precise definitions and standardized practices in surveillance strategies. Advances in technology and clinical evidence continue to shape these protocols, ensuring better patient outcomes8.
| Patient Group | Surveillance Interval |
|---|---|
| Average-risk individuals | Every 10 years starting at age 45 |
| High-risk individuals (family history) | Every 5 years, starting 10 years younger than the youngest affected relative |
| Ulcerative colitis patients | Every 1-3 years, starting 8 years after symptom onset |
| Primary sclerosing cholangitis patients | Annual surveillance |
These guidelines reflect a commitment to reducing cancer risk through tailored management and advanced diagnostic techniques. By adhering to these protocols, healthcare providers can ensure timely detection and intervention9.
High Definition White Light Endoscopy in IBD
High-definition white light endoscopy has revolutionized the detection of subtle mucosal changes in patients with chronic bowel conditions. This advanced imaging technology offers enhanced pixel density and image clarity, enabling clinicians to identify abnormalities with greater precision10.
The improved resolution of high-definition endoscopy allows for better visualization of inflammatory changes in the bowel. This is particularly useful in differentiating between benign inflammation and dysplastic lesions, which are precursors to cancer7.
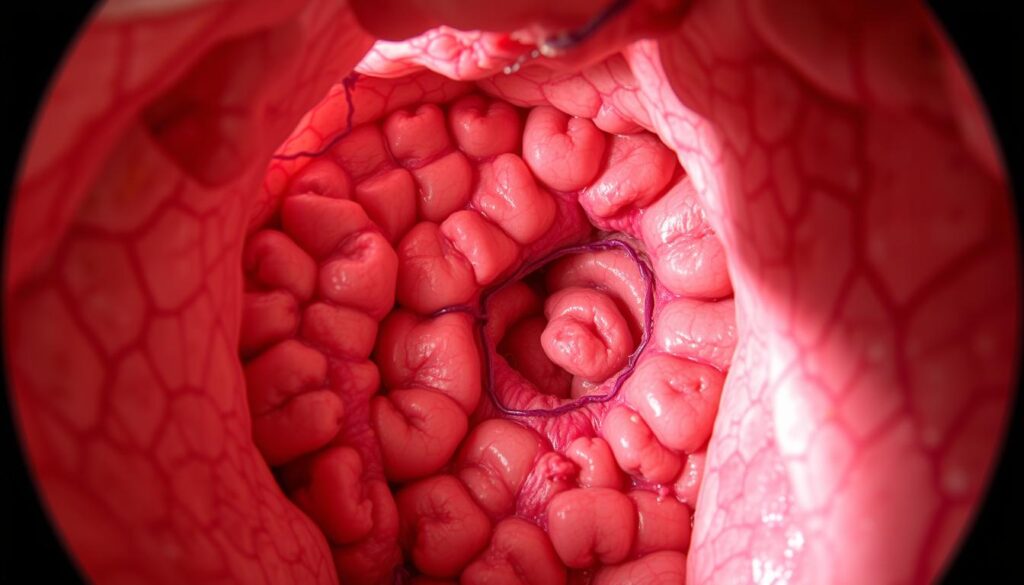
Studies have shown that high-definition imaging significantly increases adenoma detection rates compared to standard-definition systems. For example, the odds ratio for neoplasia detection with high-definition endoscopy is 1.93, highlighting its diagnostic superiority10.
Technical advancements, such as higher pixel density and improved light sources, contribute to the enhanced diagnostic accuracy of this method. These innovations ensure that even subtle mucosal lesions are detected early, reducing the risk of progression to colorectal cancer3.
| Endoscopy Type | Adenoma Detection Rate | Odds Ratio for Neoplasia Detection |
|---|---|---|
| Standard-Definition | Lower | 1.0 (Reference) |
| High-Definition | Higher | 1.93 |
In summary, high-definition white light endoscopy is a critical tool in the management of chronic bowel conditions. Its ability to detect subtle lesions and differentiate between inflammation and dysplasia makes it indispensable in modern clinical practice7.
Colonoscopy technique for IBD surveillance
Modern advancements in endoscopic imaging have transformed the way clinicians monitor patients with chronic bowel conditions. These innovations focus on improving the detection of precancerous lesions and enhancing diagnostic accuracy11.
Targeted biopsy protocols have replaced traditional random sampling methods. This approach allows for precise tissue sampling, reducing the likelihood of missed dysplasia. Studies show that targeted biopsies increase detection rates by up to 30% compared to random sampling12.
The integration of virtual chromoendoscopy has further improved diagnostic outcomes. This technology enhances mucosal visualization, making it easier to identify subtle lesions. Recent guidelines recommend its use as a standard tool in monitoring patients with chronic bowel inflammation13.
Adapting surveillance methods to individual patient needs is critical. Factors such as disease severity, inflammation extent, and family history influence the frequency and type of monitoring required11. Tailored approaches ensure timely detection and intervention.
Best practices include combining advanced imaging with targeted biopsies and regular follow-ups. These strategies support effective monitoring and early detection of abnormalities, reducing the risk of progression to colorectal cancer12.
The Role of Chromoendoscopy in Detecting Dysplasia
Chromoendoscopy has emerged as a pivotal tool in identifying precancerous changes in patients with chronic bowel inflammation. This technique uses dyes to enhance mucosal visualization, making it easier to detect subtle abnormalities14. By improving the contrast between normal and abnormal tissue, chromoendoscopy plays a critical role in dysplasia detection.
Dye-Based Techniques and Their Advantages
Dye-based chromoendoscopy involves the application of stains like methylene blue or indigo carmine to the mucosal surface. These stains enhance the visualization of surface irregularities and delineate lesion borders more effectively than traditional white light endoscopy14. Studies show that this method significantly increases the yield of dysplasia detection, particularly in patients with chronic inflammation15.
The technique is simple, quick, and cost-effective, making it widely accessible in clinical settings14. Its ability to identify invisible dysplasia, which is often missed by standard methods, underscores its diagnostic superiority10.
Comparisons with Traditional Methods
When compared to white light endoscopy, dye-based chromoendoscopy demonstrates a higher diagnostic accuracy. A meta-analysis revealed that it increases adenoma detection rates by 20% and adenomas per colonoscopy by 50%15. This improvement is particularly notable for flat or subtle lesions, which are challenging to detect with conventional methods10.
The integration of targeted biopsy protocols further enhances the precision of chromoendoscopy. By focusing on suspicious areas, clinicians can reduce the likelihood of missed dysplasia and improve patient outcomes14.
| Method | Adenoma Detection Rate | Advantages |
|---|---|---|
| White Light Endoscopy | Lower | Standard, widely available |
| Dye-Based Chromoendoscopy | Higher | Enhanced lesion visualization, higher dysplasia detection |
In summary, chromoendoscopy offers a significant advancement in the identification and characterization of precancerous changes. Its ability to improve mucosal visualization and integrate targeted biopsies makes it an indispensable tool in modern clinical practice10.
Virtual Chromoendoscopy: Technology and Application
Virtual chromoendoscopy represents a significant leap forward in endoscopic imaging technology. This advanced method uses digital filters to enhance mucosal visualization, eliminating the need for dye-based techniques. By improving contrast and detail, it aids in the detection of subtle lesions that might otherwise go unnoticed15.
Emerging Tools and HD iSCAN Insights
One of the most notable advancements in this field is the HD iSCAN platform. This tool combines high high-definition imaging with virtual chromoendoscopy to provide unparalleled clarity. Studies show that HD iSCAN increases lesion detection rates by up to 20% compared to traditional methods10.
The integration of HD iSCAN into clinical practice has streamlined workflows. Its ability to differentiate between normal and abnormal tissue reduces the need for unnecessary biopsies. This efficiency is particularly valuable in busy gastroenterology departments16.
Practical Implementation in Clinical Settings
Implementing virtual chromoendoscopy requires minimal additional training. Clinicians can easily switch between standard and enhanced imaging modes during procedures. This flexibility ensures that even subtle abnormalities are identified without disrupting the workflow15.
Cost-effectiveness is another advantage. Unlike dye-based methods, virtual chromoendoscopy does not require additional consumables. This makes it a sustainable option for long-term use in gastroenterol hepatol practices10.
“Virtual chromoendoscopy has revolutionized our ability to detect early-stage abnormalities, offering a non-invasive yet highly effective solution.”
In summary, virtual chromoendoscopy is transforming the way clinicians approach endoscopic imaging. Its integration of high high-definition technology and practical implementation strategies ensures better patient outcomes and operational efficiency16.
Biopsy Strategies: Targeted vs. Random
Effective biopsy strategies are critical in identifying precancerous changes in patients with chronic bowel inflammation. Targeted biopsie protocols, combined with advanced imaging, have become the preferred method for detecting dysplasia. This approach focuses on sampling specific areas of concern, improving diagnostic accuracy17.
In contrast, random biopsie methods involve taking tissue samples from multiple areas without specific targeting. While historically common, this approach has limitations. Studies show that random sampling often misses subtle lesions, leading to delayed diagnoses18.
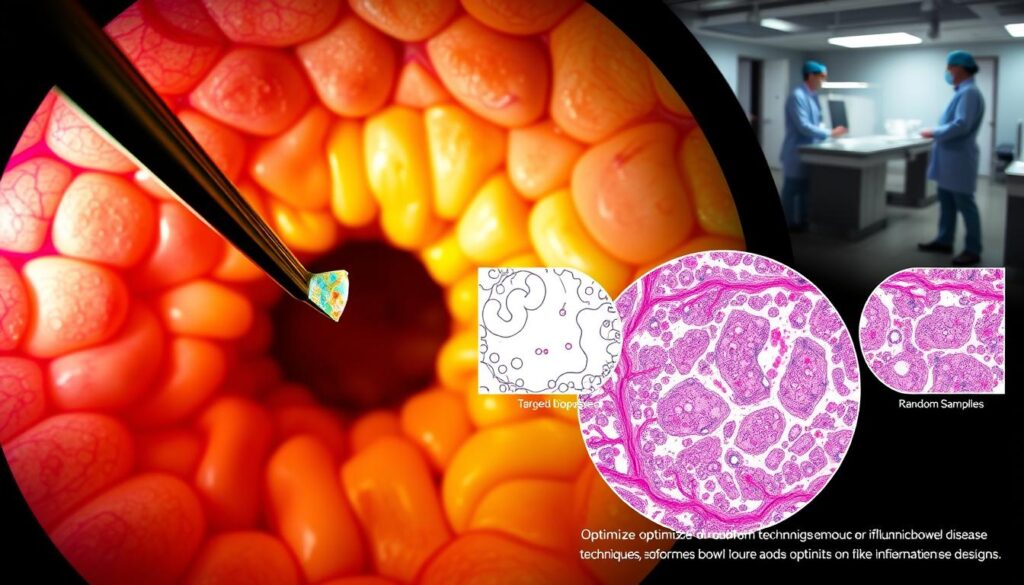
Clinical evidence supports the superiority of targeted biopsie strategies. For example, targeted sampling increases dysplasia detection rates by up to 30% compared to random methods17. This precision is particularly valuable in patients with crohn colitis, where inflammation can obscure abnormalities.
However, random biopsie protocols may still be warranted in high-risk cases. Patients with primary sclerosing cholangitis or extensive inflammation may benefit from additional sampling to ensure no lesions are missed18.
The practical impact of these findings is significant. By adopting targeted biopsie strategies, clinicians can reduce procedure times and improve patient outcomes. This approach aligns with current guidelines, emphasizing precision in monitoring chronic bowel conditions17.
Managing Visible and Invisible Dysplasia in IBD
Effective management of dysplasia in patients with chronic bowel conditions requires precise endoscopic techniques and structured follow-up strategies. Both visible and invisible lesions pose significant challenges, necessitating tailored approaches to reduce cancer risk19.
Endoscopic Resection Techniques
Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are widely used for removing visible dysplasia. These techniques allow for complete removal of precancerous lesions, reducing the likelihood of progression to colorectal cancer16.
Studies show that EMR and ESD significantly improve long-term outcomes. For example, complete resection rates exceed 90%, with recurrence rates as low as 5% in some cases19. These methods are particularly effective for flat or subtle lesions that are challenging to detect with traditional techniques16.
Risk Assessment and Follow-up Strategies
Risk stratification is critical in determining follow-up intervals. Patients with high-risk factors, such as extensive inflammation or a family history of colorectal neoplasia, require more frequent monitoring19.
Structured follow-up protocols ensure timely detection of recurrent or new lesions. For example, patients with complete resection of dysplasia should undergo surveillance every 6-12 months, depending on individual risk factors16.
| Risk Factor | Follow-up Interval |
|---|---|
| Low-risk patients | Every 12 months |
| High-risk patients | Every 6 months |
| Post-resection monitoring | Every 6-12 months |
Integrating risk evaluation with management protocols is essential for reducing cancer risk. By adhering to these strategies, clinicians can ensure better patient outcomes and minimize the progression of colorectal neoplasia19.
Surveillance Strategies for High-risk IBD Patients
Patients with primary sclerosing cholangitis and extensive colitis require tailored monitoring strategies due to their elevated cancer risk. These individuals represent a particularly high-risk group for colorectal neoplasia, necessitating intensified surveillance protocols13.
Special Considerations for PSC and Extensive Disease
Updated guidelines emphasize the need for shorter surveillance intervals in high-risk patients. Those with primary sclerosing cholangitis should undergo annual monitoring, while individuals with extensive colitis require screenings every 1-3 years20.
Risk stratification plays a critical role in designing individualized protocols. Factors such as disease duration, severity, and family history of colorectal neoplasia influence the frequency and intensity of surveillance13.
Dye-based chromoendoscopy has demonstrated superior neoplasia detection in patients with primary sclerosing cholangitis and colitis. This technique enhances mucosal visualization, improving the identification of subtle lesions21.
| Patient Group | Surveillance Interval |
|---|---|
| Primary Sclerosing Cholangitis | Annual |
| Extensive Colitis | Every 1-3 years |
| High-risk (Family History) | Every 1-2 years |
Tailored approaches ensure timely detection and intervention, reducing the progression of colorectal neoplasia. By adhering to these protocols, clinicians can improve outcomes for high-risk patients20.
Integrating New Technologies in Endoscopic Surveillance
Emerging technologies are reshaping the landscape of endoscopic monitoring for chronic bowel conditions. Innovations like AI and virtual chromoendoscopy are setting new standards in diagnostics, enhancing the precision of surveillance protocols22.
Recent advancements in imaging modalities have significantly improved the accuracy of screenings. For example, the Paddington International Virtual ChromoendoScopy ScOre (PICaSSO) demonstrates a sensitivity of 89.8% and specificity of 95.7%, making it a reliable tool for predicting histological remission22.
These technologies integrate seamlessly with existing endoscopic procedures. Enhanced imaging techniques, such as Texture and Colour Enhancement Imaging (TXI), provide detailed mucosal visualization, improving the detection of subtle lesions22.
Clinical evidence supports the adoption of these innovations. Studies show that virtual chromoendoscopy increases adenoma detection rates by up to 20%, surpassing traditional methods23. This advancement is particularly valuable in high-risk patients, where early detection is critical.
| Technology | Advantages | Clinical Impact |
|---|---|---|
| Virtual Chromoendoscopy | Enhanced lesion visualization | Higher dysplasia detection rates |
| AI Integration | Improved diagnostic accuracy | Reduced procedure times |
| Enhanced Imaging | Detailed mucosal analysis | Early detection of abnormalities |
The implications for gastroenterology practice are profound. By adopting these technologies, clinicians can improve patient outcomes and reduce the risk of progression to colorectal cancer22.
In summary, the integration of new technologies in endoscopic surveillance is transforming clinical practice. These advancements ensure more accurate screenings and better risk assessment, ultimately enhancing patient care23.
Clinical Practice Updates and Future Guidelines
Recent advancements in clinical guidelines are reshaping the approach to monitoring chronic bowel conditions. These updates emphasize precision in diagnosis and standardized assessment of lesions, ensuring better patient outcomes24.
Forthcoming recommendations highlight the importance of evidence-based updates to current protocols. For example, the 2024 ACG/ASGE Position Statement introduces new performance targets, such as a 90% threshold for adequate bowel preparation24. These changes aim to improve the accuracy of diagnosis and reduce risk factors.
Clinical articles underscore the need for continuous improvement in monitoring strategies. Studies show that the adenoma detection rate (ADR) should exceed 50% for positive screening tests, reflecting the evolving standards in gastroenterology24.
Standardized assessment of lesions is critical in reducing cancer risk. The Boston Bowel Preparation Scale (BBPS) is now preferred for evaluating preparation quality, ensuring consistent visualization of the colon24.
These updates are expected to influence clinical practice significantly. By integrating advanced tools and adhering to revised guidelines, clinicians can enhance diagnostic accuracy and patient care25.
Future directions include the adoption of AI and enhanced imaging techniques. These innovations promise to further improve diagnosis and streamline workflows in gastroenterology7.
Case Studies and Real-World Outcomes
Real-world case studies demonstrate the effectiveness of advanced diagnostic tools in improving patient outcomes. These examples highlight how optimized endoscopic methods enhance dysplasia detection and contribute to better management of chronic bowel conditions.
Illustrative Success Stories in Dysplasia Detection
One notable case involved a patient with extensive crohn colitis who underwent targeted surveillance. Advanced imaging identified invisible lesions, leading to early intervention and successful resection. This approach reduced the risk of progression to colorectal cancer26.
Another clinical scenario showcased the benefits of multidisciplinary care. A team of gastroenterologists, radiologists, and pathologists collaborated to manage a patient with colorectal neoplasia. Their combined expertise ensured accurate diagnosis and timely treatment27.
- Advanced imaging techniques improve dysplasia detection in high-risk patients.
- Targeted surveillance protocols enhance early identification of lesions.
- Multidisciplinary teams play a critical role in achieving favorable outcomes.
These case studies underscore the importance of tailored monitoring strategies. By integrating advanced tools and collaborative care, clinicians can significantly improve patient outcomes and reduce the burden of colorectal cancer.
Education and Training in IBD Endoscopy
Achieving proficiency in identifying precancerous changes requires structured education and hands-on training. Endoscopists specializing in chronic bowel conditions must undergo rigorous programs to enhance diagnostic accuracy and improve patient outcomes28.
Training protocols emphasize practical experience in dysplasia detection. GI fellows are required to complete a 3-year fellowship, including a minimum of 18 months of clinical training28. This ensures they gain the necessary skills to interpret advanced imaging techniques effectively.
Key factors contributing to enhanced diagnostic accuracy include exposure to a high volume of procedures. For example, trainees must perform at least 140 colonoscopies and 130 esophagogastroduodenoscopies to meet competency thresholds28.
Developing Proficiency in Lesion Identification
Structured feedback and mentorship are critical components of training. Programs often include interactive sessions and real-time case studies to reinforce learning29. This approach helps trainees develop the confidence to identify subtle abnormalities in colitis patients.
Emerging technologies, such as AI-assisted imaging, are increasingly integrated into training curricula. These tools standardize endoscopic grading and improve the detection of mucosal inflammation30. Trainees learn to leverage these advancements for better risk assessment.
| Procedure | Minimum Required Cases |
|---|---|
| Colonoscopy | 140 |
| Esophagogastroduodenoscopy | 130 |
| Flexible Sigmoidoscopy | 25–30 |
| Endoscopic Retrograde Cholangiopancreatography | 180–200 |
Continuous learning is essential for maintaining expertise. After fellowship, endoscopists must stay updated on evolving guidelines and technological advancements28. This commitment to education ensures they provide the highest standard of care in clinical practice.
Role of Multidisciplinary Teams in IBD Management
Multidisciplinary teams play a pivotal role in managing complex cases of chronic bowel inflammation and associated neoplasia. These teams bring together diverse expertise to enhance diagnostic accuracy and improve patient outcomes31.
The integration of gastroenterologists, colorectal surgeons, and pathologists ensures a comprehensive approach to management. Each specialist contributes unique insights, enabling precise identification and treatment of precancerous changes32.
Collaborative efforts are particularly effective in improving dysplasia detection. For example, gastroenterologists focus on endoscopic evaluation, while pathologists provide detailed histological analysis. This synergy reduces the likelihood of missed lesions and ensures timely intervention31.
Shared decision-making is another key benefit of multidisciplinary teams. By combining their expertise, specialists can tailor management strategies to individual patient needs. This approach is especially valuable for high-risk cases, where personalized care is essential32.
Weekly interdisciplinary conferences further enhance patient care. These meetings allow specialists to discuss complex cases and develop consensus treatment plans. Such coordination ensures that all aspects of patient inflammatory conditions are addressed comprehensively31.
| Specialist | Role |
|---|---|
| Gastroenterologist | Endoscopic evaluation and monitoring |
| Colorectal Surgeon | Surgical intervention for advanced cases |
| Pathologist | Histological analysis of tissue samples |
In summary, multidisciplinary teams are essential for optimizing management of chronic bowel conditions. Their collaborative approach improves diagnostic accuracy, enhances patient care, and reduces the risk of progression to cancer32.
Conclusion
Optimizing diagnostic strategies for chronic bowel conditions has become a cornerstone in reducing cancer risk. Advanced tools like high-definition imaging and targeted biopsie protocols have significantly improved diagnosis accuracy. These innovations allow for earlier detection of abnormalities, enhancing management outcomes.
Risk assessment remains critical in tailoring monitoring intervals. Multidisciplinary teams, including gastroenterologists and pathologists, play a pivotal role in ensuring comprehensive care. Their collaborative approach improves patient inflammatory condition outcomes and reduces the likelihood of missed lesions.
Future advancements, such as AI integration, promise to further refine diagnostic practices. Continued research and training are essential to maintain the highest standards in clinical care. By adopting these strategies, healthcare providers can ensure better outcomes for patients with chronic bowel conditions33.
FAQ
What is the role of colonoscopy in managing inflammatory bowel disease?
Colonoscopy plays a critical role in detecting dysplasia and colorectal cancer in patients with inflammatory bowel disease. It allows for early intervention and improved outcomes.
How does primary sclerosing cholangitis affect colorectal cancer risk in IBD patients?
Primary sclerosing cholangitis significantly increases the risk of colorectal cancer in patients with inflammatory bowel disease, necessitating more frequent and detailed surveillance.
What are the current guidelines for surveillance colonoscopy in IBD?
Current guidelines recommend regular surveillance colonoscopy for IBD patients, with intervals tailored to individual risk factors such as disease extent, duration, and presence of primary sclerosing cholangitis.
How does chromoendoscopy improve dysplasia detection in IBD?
Chromoendoscopy enhances dysplasia detection by using dye-based techniques to highlight abnormal tissue, providing better visualization compared to traditional white light endoscopy.
What is the difference between targeted and random biopsies in IBD surveillance?
Targeted biopsies focus on visible lesions, while random biopsies sample areas without visible abnormalities. Targeted biopsies are more effective in detecting dysplasia in IBD patients.
What advancements have been made in endoscopic imaging for IBD?
Advancements include high-definition white light endoscopy, virtual chromoendoscopy, and dye-based techniques, all of which improve the detection of dysplasia and colorectal cancer in IBD patients.
How often should high-risk IBD patients undergo surveillance colonoscopy?
High-risk IBD patients, such as those with primary sclerosing cholangitis or extensive disease, should undergo surveillance colonoscopy annually or as recommended by their healthcare provider.
What are the key recommendations from international societies for IBD surveillance?
International societies recommend using advanced imaging techniques like chromoendoscopy, tailored surveillance intervals, and a multidisciplinary approach to manage IBD-related colorectal cancer risk.
How can multidisciplinary teams improve IBD management?
Multidisciplinary teams, including gastroenterologists, surgeons, and pathologists, enhance IBD management by providing comprehensive care, improving diagnostic accuracy, and optimizing treatment strategies.
What training is required for proficiency in IBD endoscopy?
Proficiency in IBD endoscopy requires specialized training in advanced imaging techniques, dysplasia identification, and the use of technologies like chromoendoscopy and virtual chromoendoscopy.
Source Links
- Management of Colorectal Neoplasia in IBD Patients: Current Practice and Future Perspectives – https://pmc.ncbi.nlm.nih.gov/articles/PMC11479698/
- From random to precise: updated colon cancer screening and surveillance for inflammatory bowel disease – https://tgh.amegroups.org/article/view/8700/html
- Water-assisted colonoscopy in inflammatory bowel diseases: From technical implications to diagnostic and therapeutic potentials – https://www.wjgnet.com/1948-5190/full/v16/i12/647.htm
- Inflammatory bowel disease, colitis, and cancer: unmasking the chronic inflammation link – https://pmc.ncbi.nlm.nih.gov/articles/PMC11513726/
- Surveillance Colonoscopy Findings in Older Adults With a History of Colorectal Adenomas – https://pmc.ncbi.nlm.nih.gov/articles/PMC10988351/
- Screening and Surveillance of Colorectal Cancer: A Review of the Literature – https://pmc.ncbi.nlm.nih.gov/articles/PMC11312202/
- Best Practices for Dysplasia Detection, Surveillance and Management in IBD – Practical Gastro – https://practicalgastro.com/2024/08/05/best-practices-for-dysplasia-detection-surveillance-and-management-in-ibd/
- PDF – https://www.uhcprovider.com/content/dam/provider/docs/public/policies/oxford/Oxford-Colonoscopy-Guidelines-08-01-2024.pdf
- ECCO Guidelines on Inflammatory Bowel Disease and Malignancies – https://hal.sorbonne-universite.fr/hal-04879033/document
- Dye-based chromoendoscopy detects more neoplasia than white light endoscopy in patients with primary sclerosing cholangitis and IBD – https://pmc.ncbi.nlm.nih.gov/articles/PMC11555309/
- Ulcerative colitis – Diagnosis and treatment – https://www.mayoclinic.org/diseases-conditions/ulcerative-colitis/diagnosis-treatment/drc-20353331
- Overview of colonoscopy in adults – https://www.uptodate.com/contents/overview-of-colonoscopy-in-adults
- Surveillance colonoscopy in PSC-IBD: Some answers but more questions remain – https://pmc.ncbi.nlm.nih.gov/articles/PMC11855249/
- Chromoendoscopy – UpToDate – https://www.uptodate.com/contents/chromoendoscopy
- PDF – https://www.blueshieldca.com/content/dam/bsca/en/provider/docs/medical-policies/Chromoendoscopy-Adjunct-Colonoscopy.pdf
- GETECCU – Grupo Español de Trabajo en Enfermedad de Crohn y Colitis Ulcerosa – https://endi.geteccu.org/ii-4-2-evidence-supporting-chromoendoscopy-in-the-screening-of-cancer-associated-with-colitis-and-its-use-in-ibd-units/
- Inflammatory Bowel Disease and Colorectal Cancer – https://pmc.ncbi.nlm.nih.gov/articles/PMC11394070/
- Diagnostic Procedures for Inflammatory Bowel Disease: Laboratory, Endoscopy, Pathology, Imaging, and Beyond – https://pmc.ncbi.nlm.nih.gov/articles/PMC11241288/
- Surgical Management of Inflammatory Bowel Disease – https://pmc.ncbi.nlm.nih.gov/articles/PMC11554358/
- Screening for colorectal cancer: Strategies in patients at average risk – https://www.uptodate.com/contents/screening-for-colorectal-cancer-strategies-in-patients-at-average-risk
- Colonoscopy and Inflammatory Bowel Disease: An Easy Guide – https://curasia.com/colonoscopy-and-inflammatory-bowel-disease-a-comprehensive-guide/
- Artificial intelligence-enabled advanced endoscopic imaging to assess deep healing in inflammatory bowel disease – https://egastroenterology.bmj.com/content/2/3/e100090
- Robotic wireless capsule endoscopy: recent advances and upcoming technologies – Nature Communications – https://www.nature.com/articles/s41467-024-49019-0
- Quality Indicators for Colonoscopy: New Targets… But Will They Be Measured? – American College of Gastroenterology – https://gi.org/journals-publications/ebgi/schoenfeld_oct2024/
- Improved Diagnosis, Management for Inflammatory Bowel Disease – https://www.uhhospitals.org/for-clinicians/articles-and-news/articles/2024/12/improved-diagnosis-management-for-inflammatory-bowel-disease
- A Treat-to-Target Approach in IBD: Contemporary Real-World Perspectives from an International Survey – https://pmc.ncbi.nlm.nih.gov/articles/PMC11818273/
- REAL-Colon: A dataset for developing real-world AI applications in colonoscopy – Scientific Data – https://www.nature.com/articles/s41597-024-03359-0
- Gastrointestinal endoscopy training in the United States: Program structure and competence assessment – https://pmc.ncbi.nlm.nih.gov/articles/PMC11227727/
- GIEQs Webinar on Surveillance of IBD – https://www.gieqs.com/pro-content/378
- AI for IBD: Will Emerging Technology Revolutionize Care? – https://www.gastroenterologyadvisor.com/features/ai-for-ibd/
- Clinical Pharmacists Play Pivotal Role in Managing Inflammatory Bowel Disease – https://www.drugtopics.com/view/clinical-pharmacists-play-pivotal-role-in-managing-inflammatory-bowel-disease
- Crohn’s and Colitis Center – https://www.massgeneral.org/digestive/treatments-and-services/crohns-colitis
- Longer Colonoscopy Withdrawal Time Is Associated With the Detection of Visible Dysplasia in Patients With Inflammatory Bowel Disease – https://pmc.ncbi.nlm.nih.gov/articles/PMC10998460/