Key Takeaways
- Understanding Post-Polypectomy Bleeding: Definition and Statistics
- Risk Factors Associated with Bleeding Complications
- Post Polypectomy Bleeding Prevention: Essential Guidelines
- Immediate vs. Delayed Bleeding: Key Differences
Colonoscopic polypectomy is a fundamental procedure in the prevention of colorectal cancer. Despite its effectiveness, it poses certain risks. Post-polypectomy bleeding, the most common complication, affects between 0.3% and 6.1% of patients1. It is imperative to comprehend and mitigate this risk to ensure patient safety and achieve optimal outcomes.
The frequency of post-polypectomy bleeding is contingent upon the timing and characteristics of the polyp. Immediate bleeding occurs in 1.5% to 2.8% of procedures, whereas delayed bleeding affects up to 2% of patients1. Polyp size is a significant determinant of risk, with larger polyps presenting greater challenges.
Prevention strategies are indispensable in mitigating bleeding risks. These encompass meticulous pre-procedure assessment, judicious selection of technique, and diligent patient monitoring. For high-risk scenarios, advanced prevention methodologies may be imperative. The management of anticoagulation in polypectomy patients necessitates particular attention to minimize complications.
Healthcare professionals must remain abreast of the most current guidelines and evidence-based practices in post-polypectomy bleeding prevention. Such knowledge is essential to guarantee the safest possible outcomes for patients undergoing this critical cancer prevention procedure.
Key Takeaways
- Post-polypectomy bleeding affects 0.3% to 6.1% of cases
- Larger polyps carry a higher risk of delayed bleeding
- Prevention strategies are critical for patient safety
- Pre-procedure assessment aids in identifying high-risk patients
- Anticoagulation management demands special consideration
- Healthcare professionals must stay updated on latest guidelines
Understanding Post-Polypectomy Bleeding: Definition and Statistics
Post-polypectomy bleeding (PPB) emerges as a critical concern within the realm of colonoscopy procedures. It manifests when blood vessels at the polypectomy site persist in bleeding post-polyp removal. This complication can manifest in two distinct forms: immediate bleeding and delayed bleeding.
Types of Post-Polypectomy Bleeding
Immediate bleeding occurs during or shortly after the procedure, often visible to the endoscopist, allowing for immediate intervention. In contrast, delayed bleeding may emerge hours to days post-procedure, posing challenges as patients may have been discharged.
Incidence Rates and Risk Factors
The incidence of PPB is influenced by various factors. Patients on antithrombotic agents exhibit a significantly heightened risk. With heparin bridge therapy, PPB rates can escalate to 20%, whereas without it, the rate diminishes to 1.4%2. Overall, PPB rates span from 1.8% to 7% when antithrombotic agents are temporarily interrupted and promptly resumed2.
Risk factors for PPB encompass polyp size, electrocautery type, patient age, polyp morphology, and antithrombotic agent use2. Chronic kidney disease and liver cirrhosis also elevate the risk3.
| Factor | Impact on PPB Risk |
|---|---|
| Heparin Bridge Therapy | Up to 20% incidence |
| No Heparin Bridge Therapy | 1.4% incidence |
| Antithrombotic Agents (interrupted) | 1.8% to 7% incidence |
Impact on Patient Outcomes
While mortality directly attributable to delayed PPB is rare, it can precipitate severe complications. These include hospitalization, repeated colonoscopy, blood transfusions, and, in extreme cases, colectomy3. The aging population and increased antithrombotic agent use have contributed to the persistent incidence of delayed PPB in recent years3.
To mitigate risks, prophylactic clipping may be advisable when the PPB rate is ≥3.4% due to anticoagulant bleeding risk or ≥2.5% due to anti-platelet bleeding risk2. Careful patient assessment and tailored management strategies are imperative in minimizing PPB and its impact on patient outcomes.
Risk Factors Associated with Bleeding Complications
Post-polypectomy bleeding (PPB) emerges as a critical concern within the realm of colonoscopy procedures. The incidence of PPB spans from 0.3% to 6.1%, with immediate bleeding manifesting in 1.5% to 2.8% of cases4. Identifying the risk factors is imperative for mitigating these complications.
Patient-Related Factors
Age significantly influences PPB risk. Individuals aged 65 years or older exhibit a heightened risk of immediate bleeding4. Body mass index (BMI) also plays a role, with those of high BMI experiencing a 3.681 times greater likelihood of delayed PPB5. Comorbidities, such as cardiovascular or chronic renal disease, further elevate bleeding risk.
Polyp Characteristics
Polyp size emerges as a critical determinant. Polyps exceeding 10 mm demonstrate a 2.605 times higher risk of delayed PPB5. The risk escalates to 6.5% for polyps surpassing 20 mm4. Pedunculated polyps exhibit a 3.517 times higher risk compared to other polyp types5. Location also influences risk, with right hemicolon polyps presenting a 3.10 times higher bleeding risk5.
Procedure-Related Factors
The selection of polypectomy technique significantly impacts bleeding risk. Techniques combining blended current and cold snaring elevate the risk of immediate bleeding4. Inadequate bowel preparation can complicate the procedure, escalating bleeding risk.
| Risk Factor | Odds Ratio | Confidence Interval |
|---|---|---|
| Polyp Size >10 mm | 2.605 | 1.035-4.528 |
| Pedunculated Polyps | 3.517 | 1.428-7.176 |
| Right Hemicolon Location | 3.10 | 1.291-5.761 |
| High BMI | 3.681 | 1.876-8.613 |
Interestingly, anticoagulant use, including non-steroidal anti-inflammatory drugs or aspirin, does not elevate the risk of delayed bleeding following polypectomy4. Yet, meticulous management of anticoagulation remains critical in high-risk patients.
Post Polypectomy Bleeding Prevention: Essential Guidelines
Implementing effective bleeding prevention guidelines is imperative to mitigate complications post-polypectomy. These protocols encompass pre-procedure evaluation, technique selection, and post-procedure monitoring, aiming to diminish risks and elevate success rates.
Pre-procedure Assessment
Conducting a meticulous pre-procedure evaluation is indispensable for identifying individuals at elevated risk of post-polypectomy hemorrhage. The dimensions and location of the polyp, alongside the patient’s medical history, are determinants of risk. Polyps exceeding 10 mm in diameter are associated with a heightened risk of delayed bleeding, with an odds ratio of 4.66. Lesions situated on the right side of the colon, most prominently in the cecum, also present increased hazards67.
Technique Selection
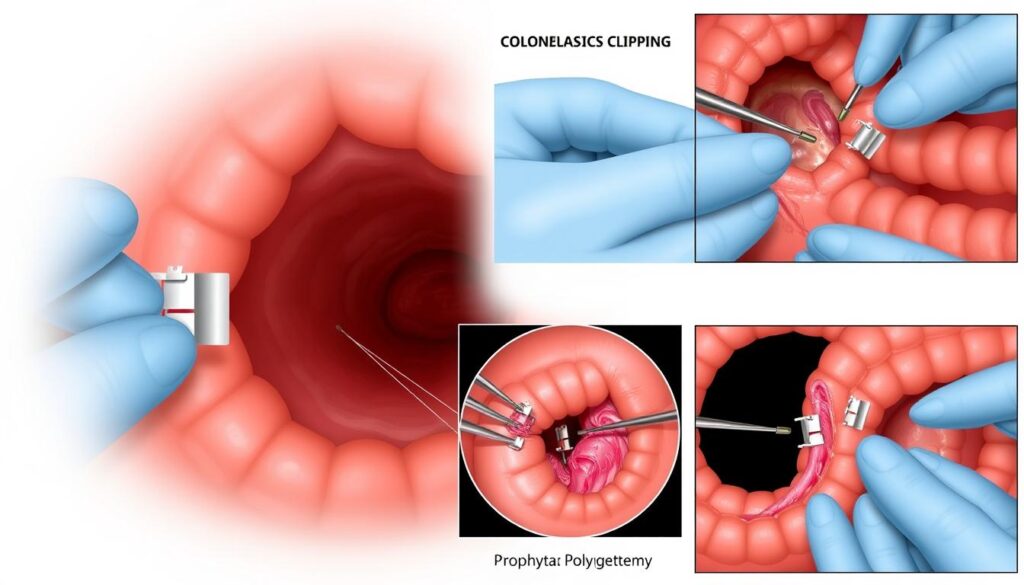
The selection of the appropriate polypectomy technique is fundamental for preventing bleeding. For polyps with a head diameter of ≥ 20 mm or a stalk diameter of ≥ 10 mm, the European Society of Gastrointestinal Endoscopy advocates for prophylactic hemostasis via adrenaline injection and/or mechanical methods like endoloops or clips. The efficacy of clipping techniques has been demonstrated, reducing delayed bleeding rates from 9.7% to 1.8%7.
Patient Monitoring Protocols
Post-procedure surveillance is of utmost importance, as delayed bleeding often manifests between several days and two weeks post-procedure7. Patients must be apprised of early warning signs and adhere to a rigorous follow-up regimen. For high-risk scenarios, such as large polyps or right-sided lesions, intensified monitoring is advisable to promptly detect and manage any bleeding episodes.
Adherence to these guidelines can significantly lower post-polypectomy bleeding rates. Research indicates that prophylactic interventions can decrease total postpolypectomy bleeding rates with high certainty of evidence8. By following these protocols, healthcare professionals can enhance patient safety and improve outcomes in polypectomy procedures.
Immediate vs. Delayed Bleeding: Key Differences
Post-polypectomy bleeding (PPB) represents a critical complication of colonoscopic interventions. It is imperative to discern the differences between immediate and delayed bleeding to implement efficacious management and preventive measures.
Characteristics of Immediate Bleeding
Immediate post-polypectomy bleeding manifests either during or immediately post-procedure. This manifestation is frequently observable to the endoscopist, enabling immediate intervention. The prevalence of immediate bleeding varies, spanning from 1.5% to 2.8% post-polypectomy.

Understanding Delayed Bleeding Patterns
Delayed post-polypectomy bleeding emerges 5 to 7 days post-procedure, though it can manifest up to 30 days thereafter. It impacts approximately 2% of patients undergoing polypectomy. An investigation involving 16,925 patients who underwent endoscopic colorectal polypectomy revealed 139 cases of postoperative bleeding, with 125 qualifying as delayed PPB9.
Time Windows for Intervention
Timely intervention is vital in managing PPB. Immediate bleeding often necessitates endoscopic hemostasis during the initial procedure. Delayed bleeding, conversely, may necessitate urgent colonoscopy for both diagnosis and treatment. A study demonstrated that post-colonoscopy hemorrhage is the primary cause of unplanned hospital admissions within a week post-procedure, underscoring the necessity for immediate action10.
Factors elevating the risk of delayed PPB include polyps exceeding 10 mm in size (OR 2.605), pedunculated polyps (OR 3.517), and those situated in the right hemicolon (OR 3.10). Elevated body mass index also augments risk (OR 3.681). These variables are instrumental in shaping intervention strategies and patient surveillance protocols11.
Advanced Prevention Techniques for High-Risk Cases
In the realm of high-risk polypectomy, the imperative for advanced prevention strategies to curtail post-procedure complications is evident. The prevalence of post-polypectomy or post-endoscopic mucosal resection (EMR) bleeding is documented to range between 1% and 7%, with a notable incidence of delayed bleeding in 4% to 7% of patients extending up to 30 days post-procedure7.
Prophylactic measures, including clip placement, have been advocated to diminish delayed post-polypectomy bleeding (DPPB) rates. For polyps of ≥2 cm, DPPB rates were significantly lower with prophylactic clipping at 4% versus 7% (pooled RR 0.55; 95% CI 0.36–0.86)12.
Advanced hemostasis techniques are of utmost importance for proximal polyps ≥2 cm, where DPPB rates were 4% with clipping versus 10% without (pooled RR 0.41; 95% CI 0.24–0.70)12. The efficacy of specific clipping techniques, such as employing clips 1 cm apart, has been demonstrated to significantly reduce delayed bleeding rates from 9.7% to 1.8%7.
| Polyp Size | Location | DPPB Rate with Clipping | DPPB Rate without Clipping |
|---|---|---|---|
| ≥2 cm | Proximal | 4% | 10% |
| ≥2 cm | Distal | No significant difference | No significant difference |
| 1-1.9 cm | Any | No significant benefit | No significant benefit |
For patients on antiplatelet or anticoagulants, DPPB rates were reduced with prophylactic clipping (pooled RR 0.50; 95% CI 0.25–0.99). The number needed to treat with clips to prevent one DPPB for polyps ≥2 cm is estimated at 23 patients12.
While prophylactic measures exhibit promise, it is critical to acknowledge that in the hands of experts, 43% of EMR sites sized ≥20 mm could not be fully closed with clips. This highlights the necessity for a customized approach in high-risk cases, taking into account polyp size, location, and patient characteristics12.
Management of Anticoagulation in Polypectomy Patients
The management of anticoagulation is of utmost importance for individuals undergoing polypectomy procedures. Given the global prevalence of over 115 million patients on clopidogrel and 33.5 million with atrial fibrillation, meticulous planning of periprocedural anticoagulation is imperative13.
Pre-procedure Medication Adjustments
Patients must undergo medication adjustments prior to polypectomy. Warfarin cessation is recommended 5 days in advance, whereas direct oral anticoagulants (DOACs) such as dabigatran, rivaroxaban, and apixaban necessitate discontinuation for 1-2 days14. Antiplatelet drugs, including clopidogrel and prasugrel, require a 7-day halt, ticagrelor a 4-day pause, and ticlopidine a 10-14 day interruption14.
Bridging Therapy Guidelines
Bridging therapy is generally not required for DOACs during warfarin interruption. Yet, for patients with high-risk conditions, low molecular weight heparin initiation 3 days prior to the procedure is advisable14. This strategy aims to mitigate thromboembolic risks while addressing bleeding concerns.
Post-procedure Anticoagulation Management
Post-procedure anticoagulation resumption necessitates precise timing. Warfarin can be reinstated on the same day if hemostasis is confirmed. DOACs are typically resumed the following day. Antiplatelet drugs should ideally be restarted within 24 hours14. The risk of postpolypectomy bleeding varies, with rates ranging from 3-11% upon antithrombotic therapy resumption13.
Optimal anticoagulation management in polypectomy patients hinges on a delicate balance between bleeding risks and thromboembolic prevention. Customized strategies, taking into account patient-specific factors and procedural nuances, are essential for achieving favorable outcomes.
Endoscopic Hemostasis Techniques
Endoscopic hemostasis is indispensable in the management of post-polypectomy bleeding, a complication that, while rare, can manifest from minor oozing to severe arterial hemorrhage15. Fortunately, the majority of instances are amenable to various endoscopic interventions15.
The arsenal of bleeding control methods encompasses mechanical, thermal, and injection modalities. Mechanical interventions include clip placement and band ligation. Thermal methods employ bipolar probes and argon plasma coagulation. Injection techniques frequently utilize epinephrine.
The selection of hemostatic devices is contingent upon the severity of bleeding, the characteristics of the polyp, and its anatomical location. Research indicates that initial hemostasis is attainable in all instances of delayed postpolypectomy bleeding (DPPB)16. Notably, approximately 7.6% of patients may experience rebleeding, typically within 3.3 days16.
Clipping emerges as a prevalent technique, with a higher number of clips required for cases at higher risk of rebleeding. The necessity of combining clipping with other modalities is underscored for complex scenarios16. Importantly, most rebleeding episodes can be managed with a single additional endoscopic procedure16.
Endoscopic mucosal resection (EMR) stands as the most commonly employed polypectomy technique, accounting for 79.5% of cases in recent studies16. This underlines the critical importance of proficiency in diverse endoscopic hemostasis techniques for effective management of bleeding.
Role of Prophylactic Clipping in Bleeding Prevention
Prophylactic clipping emerges as a critical strategy in averting post-polypectomy hemorrhage. Its utility in minimizing complications during endoscopic interventions has garnered substantial attention.
Clip Selection and Placement
The efficacy of prophylactic clipping hinges on meticulous clip placement techniques. Endoscopists meticulously choose clips, taking into account the size and location of the polyp. For polyps of considerable size, the necessity for multiple clips to achieve complete closure of the resection site becomes apparent.
Cost-Benefit Analysis
The economic viability of prophylactic clipping is a focal point. Research indicates that, despite the incremental costs associated with clip application, the prevention of bleeding events can yield substantial savings. The estimated incremental cost-effectiveness ratio stands at $15,000 per bleeding event averted17.
Evidence-Based Recommendations
Empirical evidence supports the application of prophylactic clipping in targeted scenarios. Meta-analyses reveal a notable decrease in delayed post-polypectomy bleeding (DPPB) with clip placement, most pronounced for polyps exceeding 10 mm in diameter. The incidence of DPPB was significantly lower in the hemoclip group (2.8%) compared to the standard group (5.6%) for polyps ≥10 mm18.
For polyps exceeding 2 cm, the incidence of bleeding plummeted from 12% without clips to approximately 4% with clip application17. This evidence underlines the enhanced efficacy of prophylactic clipping for larger polyps, with a particular emphasis on those situated in the proximal colon.
| Polyp Size | DPPB Risk without Clips | DPPB Risk with Clips |
|---|---|---|
| ≥10 mm | 5.6% | 2.8% |
| >20 mm | 12% | 4% |
These insights underscore the significance of selective prophylactic clipping, tailored to polyp characteristics and patient risk factors. Such an approach optimizes both bleeding prevention efficacy and resource allocation in endoscopic interventions.
Post-Procedure Monitoring and Care Protocol
Ensuring patient safety post-polypectomy necessitates a meticulous monitoring protocol. This framework delineates essential care elements following colonoscopic polypectomy interventions.
Early Warning Signs
It is imperative for patients to remain vigilant regarding bleeding indicators. These include rectal bleeding, abdominal pain, fever, and dizziness. Delayed bleeding manifestations can emerge up to 30 days post-procedure, typically manifesting between 5 to 7 days19.
Patient Education Guidelines
Education of patients is of utmost importance. It is essential to provide explicit guidance on:
- Complication recognition
- Proper wound care
- Activity limitations
- Seeking medical assistance when necessary
Follow-up Schedule
Implementing a structured follow-up regimen is critical for post-polypectomy surveillance. The recommended schedule includes:
- Phone follow-up within 24-48 hours
- Office visit at 1-2 weeks
- Final evaluation at 4-6 weeks
For individuals at higher risk, such as those on anticoagulants, intensified monitoring may be warranted. Research indicates that patients with proximal large polyps (≥20 mm) face a heightened risk of post-procedure bleeding (9.6% without preventive measures)19.
Adherence to these guidelines enables healthcare professionals to promptly identify complications, ultimately improving patient outcomes following polypectomy procedures.
Conclusion
Post-polypectomy bleeding, a pressing concern in colonoscopy, exhibits a wide range of incidence rates, from 0.4% to 10.2%20. This detailed examination of preventive measures and optimal polypectomy practices emphasizes the imperative for enhanced patient safety protocols. The adoption of cutting-edge methods, including Endoscopic Mucosal Stripping (EMS), has demonstrated efficacy in mitigating bleeding complications10.
Accurate risk assessment is fundamental in averting post-polypectomy hemorrhage. Variables such as male gender, hypertension, anticoagulant therapy, and polyp dimensions ≥ 10 mm are identified as risk factors for delayed bleeding21. Healthcare practitioners must meticulously assess these elements to craft tailored treatment strategies.
The efficacy of prophylactic clipping is a subject of ongoing discussion, with recent investigations indicating its limited effectiveness. A meta-analysis revealed no substantial disparity in bleeding incidence between cases with and without prophylactic clipping20. This underlines the necessity for continued research to enhance bleeding prevention methodologies and elevate patient outcomes in colonoscopic polypectomy procedures.
FAQ
What is post-polypectomy bleeding?
Post-polypectomy bleeding represents a complication arising post-colonoscopic polypectomy, characterized by hemorrhage from the excision site. It is categorized into immediate and delayed forms, with the latter manifesting up to 30 days post-procedure.
How common is post-polypectomy bleeding?
Incidence rates of post-polypectomy bleeding vary. Immediate bleeding affects approximately 2.8% of cases, while delayed bleeding impacts about 2%. These figures escalate in high-risk scenarios or with complex procedures.
What are the main risk factors for post-polypectomy bleeding?
Risk factors encompass patient-related elements such as advanced age and comorbidities, including cardiovascular and renal disease, alongside the use of anticoagulants or antiplatelet agents. Polyp-related factors include size, morphology, and location, with right-sided colon polyps posing a higher risk. Procedure-related factors, such as the chosen polypectomy technique and electrosurgical current settings, also influence the risk.
How can post-polypectomy bleeding be prevented?
Prevention strategies involve a thorough pre-procedure assessment and the selection of an appropriate polypectomy technique based on polyp characteristics. Patient monitoring during and after the procedure is critical, along with adherence to evidence-based guidelines. In high-risk scenarios, prophylactic clipping may be considered.
What is the difference between immediate and delayed post-polypectomy bleeding?
Immediate bleeding is observable during or immediately after the procedure, whereas delayed bleeding may occur up to 30 days post-procedure. The former is typically visible to the endoscopist, whereas the latter may present as rectal bleeding or other symptoms post-discharge. Management strategies differ between these two types of bleeding.
How should anticoagulation be managed for patients undergoing polypectomy?
Anticoagulation management necessitates careful pre-procedure medication adjustments, potentially involving temporary discontinuation of anticoagulants or antiplatelet agents. Bridging therapy may be required for high-risk patients. Post-procedure, the timing and method of resuming anticoagulation therapy must balance the risk of thromboembolic events against the risk of bleeding.
What are the main endoscopic hemostasis techniques used for post-polypectomy bleeding?
Main techniques include mechanical methods (such as clip placement and band ligation), thermal methods (such as coagulation with bipolar probes or argon plasma coagulation), and injection methods (such as epinephrine injection). Technique selection is based on bleeding severity, polyp characteristics, and anatomical location.
Is prophylactic clipping effective in preventing post-polypectomy bleeding?
The efficacy of prophylactic clipping is a subject of ongoing debate. Recent evidence suggests it may benefit proximally located colonic polyps ≥ 2 cm. Its routine use for all polypectomies is not currently recommended. The decision to employ prophylactic clipping should be based on individual patient risk factors, polyp characteristics, and resource considerations.
What should patients watch for after a polypectomy procedure?
Patients should be educated on early warning signs of post-polypectomy bleeding, including rectal bleeding, abdominal pain, fever, or signs of hypovolemia. They should be instructed on when to seek medical attention and provided with clear self-care instructions. A follow-up schedule should be established based on the patient’s risk factors and the complexity of the procedure performed.
How is post-polypectomy bleeding managed if it occurs?
Management varies based on bleeding severity and timing. Immediate bleeding is typically managed endoscopically during the procedure. Delayed bleeding may require hospitalization, blood transfusions, and repeat endoscopic procedures for hemostasis. In severe cases, interventional radiology or surgical intervention may be necessary.
Source Links
- How Do I Manage Post-Polypectomy Bleeding? – https://www.e-ce.org/journal/view.php?number=6405
- Reducing post-polypectomy bleeding events in patients who require antithrombotic agents – https://www.mayoclinic.org/medical-professionals/digestive-diseases/news/reducing-post-polypectomy-bleeding-events-in-patients-who-require-antithrombotic-agents/mac-20479873
- Effect of Instruction on Preventing Delayed Bleeding after Colorectal Polypectomy and Endoscopic Mucosal Resection – https://www.mdpi.com/2077-0383/10/5/928
- How Do I Manage Post-Polypectomy Bleeding? – https://pmc.ncbi.nlm.nih.gov/articles/PMC3429752/
- Risk Factors for Delayed Post-Polypectomy Bleeding – https://pmc.ncbi.nlm.nih.gov/articles/PMC4414758/
- Endoscopic Management of Post-Polypectomy Bleeding – https://pmc.ncbi.nlm.nih.gov/articles/PMC7280838/
- Post-polypectomy colorectal bleeding: current strategies and the way forward – https://www.e-ce.org/journal/view.php?number=7956
- Should prophylactic measures to prevent postpolypectomy bleeding after resection of large colorectal polyps be used? – https://www.medwave.cl/puestadia/resepis/6496.html?lang=en
- Frontiers | Establishment of a model for predicting delayed post-polypectomy bleeding: A real-world retrospective study – https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2022.1035646/full
- Frontiers | Postpolypectomy Bleeding Prevention and More Complete Precancerous Colon Polyp Removal With Endoscopic Mucosal Stripping (EMS) – https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2018.00312/full
- Risk Factors for Delayed Post-Polypectomy Bleeding – https://www.irjournal.org/journal/view.php?doi=10.5217/ir.2015.13.2.160
- Prevention of delayed post-polypectomy bleeding: Should we amend the 2017 ESGE Guideline? – https://pmc.ncbi.nlm.nih.gov/articles/PMC7458743/
- Antiplatelets, anticoagulants, and colonoscopic polypectomy – https://pmc.ncbi.nlm.nih.gov/articles/PMC7386094/
- Management of Antiplatelet and Anticoagulant Agents before and after Polypectomy – https://pmc.ncbi.nlm.nih.gov/articles/PMC9169436/
- Management and prevention of bleeding after colonoscopy with polypectomy – https://www.uptodate.com/contents/management-and-prevention-of-bleeding-after-colonoscopy-with-polypectomy
- Clinical outcome of endoscopic management in delayed postpolypectomy bleeding – https://www.irjournal.org/journal/view.php?doi=10.5217/ir.2017.15.2.221
- Prevention of delayed post-polypectomy bleeding by prophylactic clipping after endoscopic colorectal polypectomy: a meta-analysis – International Journal of Colorectal Disease – https://link.springer.com/article/10.1007/s00384-022-04253-0
- Role of prophylactic hemoclip placement in prevention of delayed post-polypectomy bleeding for large colon polyps: a meta-analysis of randomized controlled trials – https://pmc.ncbi.nlm.nih.gov/articles/PMC8079868/
- Clip Closure Prevents Bleeding After Endoscopic Resection of Large Colon Polyps in a Randomized Trial – https://pmc.ncbi.nlm.nih.gov/articles/PMC8224988/
- Prophylactic clipping and post-polypectomy bleeding: a meta-analysis and systematic review – https://pmc.ncbi.nlm.nih.gov/articles/PMC5049559/
- Risk factors for delayed colorectal postpolypectomy bleeding: a meta-analysis – BMC Gastroenterology – https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-024-03251-6