Key Takeaways
- Introduction to Ulcerative Colitis and Its Trends
- Overview of Disease Trends and Data Sources
- Key Findings on Ulcerative Colitis Incidence Rates
- Methodology Behind the Trend Analysis
Inflammatory bowel disease (IBD) is a chronic condition affecting millions of Americans. It encompasses disorders like Crohn’s disease and ulcerative colitis, which cause inflammation in the digestive tract. Recent studies show that over 0.7% of Americans will be diagnosed with IBD during their lifetime1.
The prevalence of IBD in the United States is significant, with 721 cases per 100,000 person-years1. This condition impacts individuals across all age groups, though it peaks in early adulthood and stabilizes in middle age. Understanding these trends is crucial for healthcare providers to improve patient outcomes.
Epidemiologic surveillance plays a vital role in tracking IBD patterns. Data reveals disparities in prevalence among racial groups, with White individuals having the highest rates at 812 cases per 100,0001. This highlights the need for targeted interventions and awareness campaigns.
This article explores the nationwide scope of IBD, its impact on healthcare, and the importance of differentiating between its subtypes. By analyzing recent data, we aim to provide insights for clinical practice and patient care.
Key Takeaways
- Over 0.7% of Americans will be diagnosed with IBD in their lifetime.
- IBD prevalence in the U.S. is 721 cases per 100,000 person-years.
- White individuals have the highest IBD rates at 812 cases per 100,000.
- IBD peaks in early adulthood and stabilizes in middle age.
- Epidemiologic surveillance is essential for tracking IBD trends.
Introduction to Ulcerative Colitis and Its Trends
The digestive tract is often affected by chronic conditions like Crohn’s disease and ulcerative colitis. These disorders, collectively known as inflammatory bowel disease (IBD), cause persistent inflammation and significantly impact quality of life. Understanding their clinical definitions and diagnostic criteria is essential for accurate identification and management.
Accurate tracking of disease trends is crucial for public health management. Recent data shows that IBD prevalence is increasing globally, with significant variations across regions and demographics2. This highlights the need for consistent diagnostic criteria in surveillance studies to ensure reliable data collection.
Evolving trends in reported cases suggest that environmental and lifestyle factors may contribute to the rise in IBD prevalence3. Integrating epidemiological data into clinical practice can improve patient care and inform targeted interventions.
“Understanding these trends is vital for developing effective public health strategies,”
emphasizes the importance of ongoing research and data analysis.
Recent statistical findings reveal that IBD affects millions worldwide, with ulcerative colitis and Crohn’s disease accounting for a significant proportion of cases2. These insights underscore the need for continued efforts to enhance diagnostic accuracy and treatment approaches.
Overview of Disease Trends and Data Sources
Recent studies highlight significant shifts in IBD patterns across the U.S4. Over the past decade, the prevalence of this disease has shown a steady rise, with notable variations by age group and region5. Data from the National Health Interview Survey (NHIS) and CDC MMWR indicate an upward trend, emphasizing the need for accurate tracking and analysis.
Age-specific patterns reveal higher prevalence among younger individuals, particularly in early adulthood6. However, older adults also show increasing rates, suggesting a broader demographic impact. Regional disparities are evident, with northeastern states reporting higher cases compared to other areas5.
Key data sources include administrative claims and national surveys, which provide comprehensive insights into disease trends4. Reliable statistical methods, such as age-adjusted rate calculations, are essential for accurate epidemiological analysis6.
“Understanding these trends is vital for developing effective public health strategies,”
Differences in data collection methods, such as self-reported surveys versus clinical records, can introduce biases4. Addressing these challenges ensures more reliable data for guiding future research priorities.
| Age Group | Prevalence per 100,000 | Region |
|---|---|---|
| 0-17 | 122 | Northeast |
| 18-34 | 812 | Midwest |
| 35+ | 721 | South |
These findings underscore the importance of integrating epidemiological data into clinical practice. By leveraging insights from national surveys and administrative claims, healthcare providers can better address the growing impact of IBD.
Key Findings on Ulcerative Colitis Incidence Rates
Recent epidemiological research highlights significant variations in disease trends across the U.S. population7. Studies show that estimates differ substantially depending on methodology, with notable increases in certain groups. Administrative data and surveys provide distinct insights into these patterns.
Administrative claims reveal an age- and sex-standardized prevalence of 721 per 100,000 population7. In contrast, national surveys estimate higher rates, suggesting discrepancies in data collection methods. These variations underscore the need for standardized approaches in epidemiological research.
Key metrics highlight disparities across demographic groups. For instance, White individuals show higher prevalence rates compared to Black and Hispanic populations7. Such findings emphasize the importance of targeted interventions in affected communities.
| Population Group | Prevalence per 100,000 | Data Source |
|---|---|---|
| White | 812 | Administrative Claims |
| Black | 504 | National Surveys |
| Hispanic | 458 | Administrative Claims |
The statistical reliability of these studies is supported by comprehensive methodologies. Age-adjusted calculations and insurance-standardized data ensure accurate analysis8. These insights are vital for guiding clinical practice and public health strategies.
Clinical implications of higher prevalence rates in certain groups include the need for tailored treatment plans. Understanding these trends helps healthcare providers address the growing impact of chronic bowel conditions effectively9.
Methodology Behind the Trend Analysis
Analyzing disease trends requires a systematic approach to data collection and interpretation. Researchers rely on national surveys, such as the National Health Interview Survey (NHIS), to gather comprehensive data10. These surveys provide insights into prevalence and demographic variations, enabling accurate trend analysis.

Data Collection and Analysis Techniques
Data collection involves a multi-step process, including the use of administrative claims and self-reported surveys. Tools like SUDAAN software are employed to adjust for sampling design and ensure statistical accuracy10. This systematic approach minimizes biases and enhances the reliability of findings.
Year-over-year comparisons are crucial for identifying emerging trends. By analyzing data across multiple years, researchers can detect patterns and predict future outcomes11. This method is particularly useful for understanding the long-term impact of chronic conditions.
“Accurate data interpretation is the foundation of effective public health strategies,”
Statistical adjustments for factors like age and demographic variables are essential. These adjustments ensure that the data reflects the true prevalence of conditions across different populations12. Rigorous methodological frameworks further validate the findings, making them actionable for healthcare providers.
| Data Source | Key Features | Applications |
|---|---|---|
| National Surveys | Self-reported data, demographic insights | Trend identification, prevalence analysis |
| Administrative Claims | Clinical records, insurance data | Age-adjusted rates, demographic comparisons |
| SUDAAN Software | Sampling adjustments, statistical analysis | Bias minimization, data validation |
Integrating technological tools into data analysis enhances efficiency and accuracy. Large public health databases are processed using advanced algorithms, enabling researchers to handle complex datasets with ease10. This integration ensures that findings are both reliable and actionable for improving patient care.
Historical Trends in Inflammatory Bowel Disease Prevalence
Over the past few decades, the landscape of chronic bowel conditions has shifted significantly. Historical data reveal a marked increase in the prevalence inflammatory bowel disease, with notable changes in demographic patterns13. This section explores these trends, comparing past and present data to highlight key differences.
Changes Over Recent Decades
In the 1990s, the global prevalence of IBD was significantly lower, with 573,500 cases reported12. By 2021, this number had more than doubled, reaching 1,278,190 cases. This increase reflects both improved diagnostic methods and a true rise in the condition.
Administrative claims and national surveys provide complementary insights into these trends. For example, age-standardized prevalence rates (ASPR) have remained relatively stable, decreasing slightly from 118.14 to 117.2912. This suggests that while the number of cases has grown, the overall burden of the disease has not increased proportionally.
Diagnostic advancements have played a crucial role in identifying more cases. Early detection methods and increased awareness have contributed to the reported rise in prevalence inflammatory bowel disease13. Additionally, socioeconomic and environmental factors, such as urbanization and dietary changes, have influenced these trends.
| Year | Prevalence (per 100,000) | Key Observations |
|---|---|---|
| 1990 | 118.14 | Lower prevalence, limited diagnostics |
| 2021 | 117.29 | Higher cases, improved detection |
Landmark studies have documented these changes, providing a foundation for understanding the evolving nature of IBD. For instance, research highlights the convergence of rates among various demographic groups, indicating a narrowing difference in prevalence across populations9.
These findings underscore the importance of continued surveillance and research. By analyzing historical trends, healthcare providers can better address the growing impact of chronic bowel conditions and develop targeted interventions.
Regional Variations in Incidence and Prevalence
Geographic location plays a significant role in the distribution of chronic bowel conditions. Studies reveal notable differences in prevalence inflammatory patterns across U.S. regions, with urban areas often showing higher rates compared to rural settings6. These disparities highlight the influence of environmental and demographic factors on disease trends.
Differences Across U.S. Regions
Regional analyses indicate that northeastern states report higher prevalence rates compared to other areas3. For instance, urban centers like New York and Boston show elevated cases, while rural regions in the Midwest and South exhibit lower rates. This variation underscores the need for localized healthcare strategies.
Data from national surveys reveal that non-central cities also experience increased disease burden6. Factors such as population density, access to healthcare, and lifestyle differences contribute to these trends. Understanding these regional patterns is crucial for effective resource allocation.
Urban vs. Rural Disparities
Urban areas often face higher prevalence inflammatory rates due to factors like pollution, dietary habits, and stress levels3. In contrast, rural regions may have lower rates but face challenges in accessing specialized care. This imbalance highlights the need for targeted interventions in both settings.
Healthcare providers must consider these disparities when planning treatment strategies. Regional analysis not only aids in understanding disease distribution but also helps identify at-risk populations. This approach ensures better outcomes for patients across diverse geographic locations.
By leveraging datum from large-scale surveys, policymakers can develop tailored public health initiatives. Addressing regional variations is essential for reducing the overall burden of chronic bowel conditions and improving healthcare equity.
Demographic Factors Influencing Incidence Rates
Demographic factors significantly shape the distribution of chronic bowel conditions across the United States. Age, race, ethnicity, and socioeconomic status all play critical roles in determining who is most affected by these conditions. Understanding these influences is essential for developing targeted public health strategies and improving healthcare equity.
Age-Related Trends
Age is a key determinant in the prevalence of chronic bowel conditions. Older adults, particularly those aged 50 and above, show higher rates of diagnosis compared to younger populations14. This trend is supported by data indicating a 53.7% decrease in prevalence among younger adults over the past three decades15.
However, younger adults are not immune. Early adulthood remains a critical period for the onset of these conditions, with significant implications for long-term health outcomes. The interplay between aging and disease progression underscores the need for age-specific interventions.
Race, Ethnicity, and Socioeconomic Status
Racial and ethnic disparities are evident in the distribution of chronic bowel conditions. Non-Hispanic White individuals report higher prevalence rates compared to Black and Hispanic populations14. These differences may stem from genetic, environmental, and healthcare access factors.
Socioeconomic status also plays a significant role. Individuals from lower-income backgrounds often face barriers to timely diagnosis and treatment, exacerbating health disparities. Addressing these inequities requires a multifaceted approach, including improved access to care and targeted awareness campaigns.
“Understanding demographic influences is crucial for reducing health disparities and improving outcomes for all populations,”
Public health monitoring must continue to track these trends to inform policy and resource allocation. By addressing demographic factors, healthcare providers can better serve diverse communities and reduce the overall burden of chronic bowel conditions.
Healthcare Cost Trends and Economic Burden
The economic burden of chronic bowel conditions has become a significant concern for the U.S. healthcare system. In 2018, the total annual healthcare cost for IBD reached approximately $8.5 billion, with biologic therapies contributing heavily to this expenditure16. This financial strain underscores the need for cost-effective interventions and efficient resource allocation.
Impact of Biologic Therapies
Biologic therapies have revolutionized treatment approaches but come with substantial costs. In 2017, the average UC-related healthcare cost in the first year after initiating advanced therapy was estimated at $42,57916. These therapies, while effective, often lead to higher overall expenses due to their complex administration and monitoring requirements.
Despite their benefits, 75% of patients experienced treatment failure within the first 12 months of initiating first-line advanced therapy, with a median time to treatment failure of 5.1 months16. This high failure rate further escalates costs, as patients often require additional treatments or hospitalizations.
Rising Total Health Care Expenditure
The total healthcare expenditure for IBD has risen significantly over the years. A detailed breakdown reveals that prescribed medicines, inpatient services, and outpatient care are the primary cost drivers16. For example, the highest total costs across treatment failure events were attributed to dose escalation or interval shortening, amounting to $101,66816.
Historical trends show a steady increase in costs, with the age-standardized prevalence rate (ASPR) of IBD decreasing from 343 per 100,000 in 1990 to 193 per 100,000 in 201914. This paradox highlights the growing financial burden despite a decline in prevalence rates.
| Cost Component | 2018 Expenditure (in billions) |
|---|---|
| Prescribed Medicines | $3.2 |
| Inpatient Services | $2.8 |
| Outpatient Care | $2.5 |
These rising costs have significant implications for healthcare policy. Policymakers must prioritize cost-effective interventions and equitable resource allocation to mitigate the financial strain on the healthcare system. Addressing this burden is essential for improving patient outcomes and ensuring sustainable healthcare practices.
Impact of Lifestyle and Health Behaviors on IBD
Lifestyle choices play a pivotal role in managing and influencing the progression of chronic bowel conditions. Factors such as smoking, sleep patterns, and physical activity have been shown to significantly affect disease outcomes. Understanding these behaviors can help improve patient management and quality of life.
Smoking, Sleep, and Physical Activity Patterns
Smoking history is a well-documented risk factor for IBD progression. Studies indicate that individuals who smoke are more likely to experience severe symptoms and complications17. Conversely, quitting smoking has been associated with improved disease management and reduced flare-ups.
Sleep duration and quality also play a critical role. Poor sleep patterns are linked to increased inflammation and disease activity18. Ensuring adequate rest can help modulate the immune response and improve overall health outcomes.
Physical activity is another key factor. Data from the “BE-FIT-IBD” study revealed that 42.9% of individuals with IBD were physically inactive, while only 4.1% met the criteria for health-enhancing physical activity17. Regular exercise, particularly moderate-intensity aerobic and resistance training, has been shown to reduce fat mass and improve cardiovascular health19.
These lifestyle factors not only influence disease severity but also impact comorbidities such as cardiovascular disease, osteoporosis, and mental health disorders17. Addressing these behaviors through patient education and self-management strategies can lead to better clinical outcomes.
“Integrating lifestyle modifications into treatment plans is essential for improving patient outcomes and reducing the overall burden of chronic bowel conditions.”
By focusing on smoking cessation, sleep hygiene, and physical activity, healthcare providers can offer a holistic approach to managing IBD. This strategy not only addresses the disease itself but also enhances the overall well-being of the person affected.
Comparative Analysis: Ulcerative Colitis Versus Crohn’s Disease
Chronic bowel conditions, while sharing similarities, exhibit distinct clinical and therapeutic profiles. Both are classified as inflammatory bowel diseases (IBD), yet they differ significantly in their presentation, management, and long-term outcomes. Understanding these differences is crucial for accurate diagnosis and effective treatment.
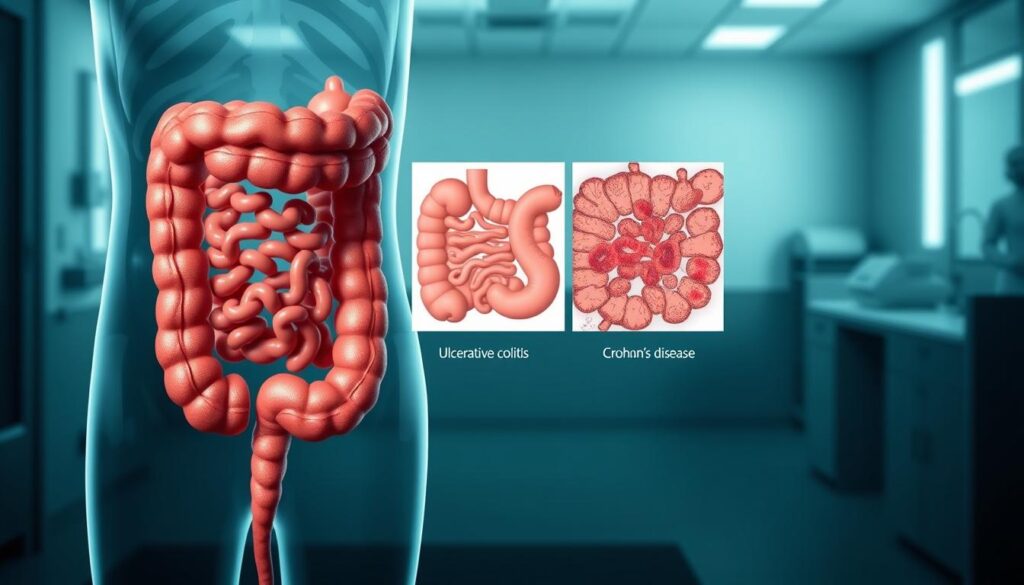
Differences in Incidence and Symptoms
Studies reveal that the occurrence of these conditions varies by region and demographic. For instance, the annual occurrence of Crohn’s disease in Europe ranges from 4.1 to 22.78 per 100,000, while ulcerative colitis ranges from 3.0 to 23.36 per 100,0009. These findings highlight the geographical and population-based disparities in disease distribution.
Symptomatology also plays a critical role in differentiation. Crohn’s disease often presents with transmural inflammation, affecting any part of the gastrointestinal tract, while ulcerative colitis is limited to the colon and rectum2. This distinction guides clinicians in making accurate diagnoses and tailoring treatment plans.
Variation in Treatment Approaches
Therapeutic strategies for these conditions differ based on disease severity and patient response. For example, biologic therapies are commonly used for Crohn’s disease, with a median time to treatment failure of 5.1 months2. In contrast, ulcerative colitis management often focuses on achieving and maintaining remission through a combination of medications and lifestyle modifications.
Key factors influencing treatment decisions include:
- Disease location and extent
- Patient age and overall health
- Response to initial therapies
These variations underscore the importance of personalized care in managing chronic bowel conditions effectively.
“Understanding the nuances between these conditions is essential for optimizing patient outcomes and reducing the overall disease burden.”
By leveraging robust data and clinical insights, healthcare providers can better navigate the complexities of these conditions. This approach ensures that patients receive the most appropriate and effective care throughout their life.
Current U.S. Prevalence and Health Data Analysis
The National Health Interview Survey (NHIS) provides critical insights into the prevalence of chronic bowel conditions in the U.S. Recent data reveals that approximately 3.1 million American adults have been diagnosed with these conditions, highlighting their significant impact on public health9.
NHIS-based Findings
The NHIS employs a robust methodology to collect and analyze data on chronic bowel conditions. This includes self-reported surveys and demographic subgroup analysis, ensuring comprehensive coverage9. The survey’s design allows for accurate tracking of trends and variations across different populations.
Key findings from the NHIS indicate notable demographic disparities. For instance, prevalence rates vary significantly by age, with older adults showing higher rates compared to younger individuals14. Regional differences are also evident, with urban areas reporting higher cases than rural settings9.
Precise figures from the NHIS show that the age-standardized prevalence rate (ASPR) for chronic bowel conditions has decreased from 343 per 100,000 in 1990 to 193 per 100,000 in 201914. This decline reflects improved diagnostic methods and targeted interventions.
The significance of NHIS data extends beyond statistical analysis. It serves as a vital tool for monitoring public health trends and guiding resource allocation. By leveraging this data, healthcare providers can develop targeted strategies to address the growing burden of chronic bowel conditions.
“Understanding demographic and regional variations is essential for reducing health disparities and improving outcomes for all populations,”
Statistical reliability is a cornerstone of NHIS findings. Age-adjusted calculations and rigorous methodological frameworks ensure the accuracy of the data3. These insights are invaluable for informing clinical practice and public health policy.
In conclusion, the NHIS offers a comprehensive view of chronic bowel conditions in the U.S. Its data-driven approach provides critical insights for addressing the challenges posed by these conditions and improving patient care.
Emerging Trends from Recent Studies
Emerging research highlights transformative shifts in the management of chronic bowel conditions. Recent studies reveal that innovative therapies, including biologics and small molecules, are reshaping treatment paradigms and influencing disease outcomes20.
Innovative Treatment Impacts
New therapeutic options are significantly altering the landscape of care. For instance, the use of biologics in patients with Crohn’s disease increased from 11.9% in 2010 to 36.6% in 201820. This shift reflects the growing reliance on advanced therapies to achieve better clinical outcomes.
Pilot studies and clinical trials indicate potential reductions in morbidity and mortality. A 2021 Italian observational study showed a rise in medical salvage therapy from 14% to 91.6% of presenting patients over a 12-year period21. These findings underscore the effectiveness of cutting-edge treatments in improving patient prognosis.
Estimates suggest that the annual occurrence of ulcerative colitis increased from 5.3 per 105 in 2010 to 8.2 per 105 in 2018, reflecting a 0.4% annual increase20. This trend highlights the growing burden of the condition and the need for continued innovation in treatment strategies.
“The integration of novel therapies into clinical practice is essential for addressing the evolving challenges of chronic bowel conditions,”
Systematic reviews and recent clinical trials provide valuable insights into future disease trends. For example, the use of immunomodulators in ulcerative colitis patients rose from 13.1% in 2010 to 16.8% in 201820. These advancements are expected to further reduce hospitalization and surgery rates.
| Treatment | Usage Increase (2010-2018) |
|---|---|
| Biologics (Crohn’s Disease) | 11.9% to 36.6% |
| Immunomodulators (Ulcerative Colitis) | 13.1% to 16.8% |
| Medical Salvage Therapy | 14% to 91.6% |
These advancements not only improve patient outcomes but also reduce the economic burden on healthcare systems. By leveraging data-driven insights, healthcare providers can better address the challenges posed by chronic bowel conditions.
Implications for Patient Care and Public Health Policy
Effective management of chronic bowel conditions requires addressing both patient care and public health policy. Rising cases of these conditions have significant practical ramifications, particularly for adult populations. Disparities in access to quality healthcare remain a critical issue, with vulnerable groups often facing barriers to timely diagnosis and treatment22.
Addressing Health Disparities
Studies reveal that Black, Asian, and Hispanic ethnic groups experience poorer health outcomes compared to their White counterparts22. Socioeconomic factors, such as income and education, further exacerbate these disparities. For instance, 12 out of 51 studies identified inequalities driven by socioeconomic differences22.
Rural populations also face unique challenges, with limited access to specialized care and higher rates of avoidable emergency admissions22. Addressing these disparities requires targeted interventions, including improved healthcare access and awareness campaigns.
Resource Allocation Strategies
Efficient resource allocation is essential to reduce the overall health burden. Data-driven strategies, such as prioritizing high-prevalence regions and underserved populations, can optimize resource distribution. For example, Michigan has the highest age-standardized incidence rate at 31 per 100,000, highlighting the need for focused interventions14.
Key strategies include:
- Expanding healthcare infrastructure in rural areas
- Increasing funding for advanced therapies
- Enhancing patient education and self-management programs
“Understanding demographic and regional variations is essential for reducing health disparities and improving outcomes for all populations,”
Policy implications based on comprehensive public health data are crucial. For instance, the age-standardized prevalence rate decreased from 343 per 100,000 in 1990 to 193 per 100,000 in 2019, reflecting improved diagnostic methods and targeted interventions14. Policymakers must leverage these insights to develop equitable and sustainable healthcare solutions.
By integrating detailed statistical analyses into clinical practice, healthcare providers can better address gaps in healthcare delivery. Evidence-based recommendations, such as prioritizing biologics for severe cases, can further improve patient outcomes23.
Advances in Data Analytics for IBD Research
Advances in data analytics are transforming the landscape of IBD research. The integration of machine learning and modern computational techniques has revolutionized how researchers analyze disease trends and treatment outcomes24. These innovations provide deeper insights into the systematic review of data, enabling more accurate predictions and tailored interventions.
Integrating Technology in Trend Analysis
Traditional data analysis methods often relied on manual processes and limited datasets. In contrast, advanced analytics tools now utilize machine learning algorithms to process large-scale data with greater precision24. For example, Random Forest models have achieved an accuracy of over 0.98 in identifying key biomarkers for IBD24.
These tools enhance the granularity of data, allowing researchers to examine trends at a more detailed level. This is particularly valuable for understanding regional variations in disease prevalence and treatment outcomes25. By leveraging these technologies, healthcare providers can develop more targeted strategies for patient care.
Case studies demonstrate the practical applications of these advancements. For instance, a recent study identified novel biomarkers like DENND2B and PANK1, which showed strong diagnostic potential24. Such findings highlight the potential for early detection and personalized treatment approaches.
| Method | Accuracy | Application |
|---|---|---|
| Random Forest | > 0.98 | Biomarker Identification |
| Support Vector Machines | 0.887 | Diagnostic Validation |
| LASSO Regression | 0.734 | Gene Expression Analysis |
The integration of these technologies into epidemiological research has significantly improved the reliability of data. For example, high-throughput transcriptomic microarray technologies have enabled the exploration of gene expression profiles with unprecedented detail24. This has led to a better understanding of the underlying mechanisms of IBD.
“The use of advanced analytics is essential for refining future research methodologies and improving patient outcomes,”
By combining traditional methods with modern computational techniques, researchers can address the complexities of chronic bowel conditions more effectively. This approach not only enhances the accuracy of data but also provides actionable insights for clinical practice.
Scientific Research and Future Directions in IBD
Scientific advancements in IBD research are paving the way for groundbreaking treatments and improved patient outcomes. Ongoing studies and clinical trials are focusing on novel therapeutics and biomarkers, which promise to revolutionize the management of this chronic condition. These efforts are driven by the need to address the limitations of current treatments and improve long-term prognosis.
Ongoing Clinical Trials and Studies
Recent clinical trials have explored the efficacy of advanced therapies, including biologics and small molecules. For instance, ustekinumab has been shown to be superior or at least non-inferior to vedolizumab as a second-line therapy after anti-TNF failure26. These findings highlight the potential of newer treatments to address unmet needs in IBD management.
Multi-center trials play a crucial role in shaping evidence-based practices. The PROFILE study, for example, demonstrated that the PredictSURE blood test was not able to accurately predict disease course26. Such studies provide valuable insights into the limitations of current diagnostic tools and the need for further innovation.
Factors Contributing to Improved Prognosis
Several scientific factors are contributing to improvements in disease prognosis. Non-invasive monitoring methods, such as fecal calprotectin and bowel ultrasound, are increasingly replacing more invasive endoscopies26. These advancements not only enhance patient comfort but also improve diagnostic accuracy.
Collaborative research efforts are also driving progress. The COVID-19 pandemic has accelerated the adoption of telemedicine, providing patients with greater choice and reducing carbon emissions26. This shift underscores the importance of integrating technology into patient care.
“The integration of novel therapies into clinical practice is essential for addressing the evolving challenges of chronic bowel conditions,”
Looking ahead, the focus will remain on developing personalized treatment strategies and improving access to care. By leveraging data-driven insights and fostering collaboration, the scientific community aims to reduce the overall burden of IBD and enhance patient outcomes.
Conclusion
The growing prevalence of chronic bowel conditions underscores the need for comprehensive data analysis and targeted interventions. Recent studies highlight significant variations in disease trends, emphasizing the importance of incorporating robust data from national surveys and clinical studies7.
These findings have critical implications for clinical practice and public health policy. By leveraging accurate data, healthcare providers can develop tailored strategies to address disparities and improve patient outcomes. Continued surveillance is essential to monitor emerging trends and guide resource allocation effectively.
Future research must focus on refining diagnostic methods and exploring innovative treatments. This approach will ensure that healthcare systems are equipped to manage the increasing burden of these conditions. Policymakers and medical professionals must collaborate to implement evidence-based solutions that enhance care and reduce health inequities.
FAQ
What is inflammatory bowel disease (IBD)?
Inflammatory bowel disease (IBD) is a chronic condition that includes ulcerative colitis and Crohn’s disease. It causes inflammation in the digestive tract, leading to symptoms like abdominal pain, diarrhea, and weight loss.
Why is tracking disease trends important?
Monitoring trends helps identify changes in disease prevalence, understand risk factors, and improve healthcare strategies. It also aids in resource allocation and policy development.
How are data sources used in IBD research?
Researchers rely on national health surveys, hospital records, and population studies to gather information on disease prevalence, incidence, and demographic patterns.
What are the key findings on ulcerative colitis trends?
Studies show that ulcerative colitis prevalence has increased over time, with higher rates observed in urban areas and among certain age groups.
What methods are used to analyze disease trends?
Data collection involves systematic reviews, statistical modeling, and population-based studies. Advanced analytics help identify patterns and predict future trends.
How has IBD prevalence changed over recent decades?
The prevalence of IBD has risen significantly, particularly in developed countries. This increase is linked to environmental and lifestyle factors.
Are there regional differences in IBD rates?
Yes, incidence and prevalence vary across U.S. regions, with urban areas often reporting higher rates compared to rural areas.
How do demographic factors influence IBD?
Age, race, ethnicity, and socioeconomic status play a role in disease risk. Younger adults and certain ethnic groups are more likely to be affected.
What is the economic burden of IBD?
IBD imposes significant healthcare costs, driven by hospitalizations, medications, and lost productivity. Biologic therapies contribute to rising expenditures.
How do lifestyle choices impact IBD?
Smoking, poor sleep, and lack of physical activity can worsen symptoms and increase disease risk. Healthy behaviors may help manage the condition.
How does ulcerative colitis differ from Crohn’s disease?
Ulcerative colitis affects the colon, while Crohn’s disease can involve any part of the digestive tract. Symptoms and treatment approaches vary between the two.
What does current U.S. health data reveal about IBD?
Data from the National Health Interview Survey (NHIS) indicates a growing prevalence of IBD, with significant impacts on patient quality of life.
What are the latest trends in IBD treatment?
Recent studies highlight the effectiveness of biologic therapies and personalized medicine in improving outcomes for patients with IBD.
How can public health policies address IBD disparities?
Policies should focus on improving access to care, reducing health inequities, and increasing funding for research and treatment.
What role does technology play in IBD research?
Advanced data analytics and digital tools enhance trend analysis, enabling more accurate predictions and tailored treatment strategies.
What are the future directions in IBD research?
Ongoing clinical trials and studies aim to uncover new therapies, understand disease mechanisms, and improve patient care.
Source Links
- IBD Statistics – https://www.gastroenterologyadvisor.com/factsheets/ibd-statistics/
- Recent trends in the epidemiology and clinical outcomes of inflammatory bowel disease in South Korea, 2010-2018 – https://www.wjgnet.com/1007-9327/full/v30/i9/1154.htm
- Global, regional, and national burden of inflammatory bowel disease, 1990–2021: Insights from the global burden of disease 2021 – International Journal of Colorectal Disease – https://link.springer.com/article/10.1007/s00384-024-04711-x
- IBD Etiology and Outcomes (CDC-Funded Program, 2018-2024) – https://www.cdc.gov/inflammatory-bowel-disease/programs/etiology-and-outcome-of-inflammatory-bowel-disease.html
- More than 100,000 young people in the US live with inflammatory bowel disease – https://www.news-medical.net/news/20241122/More-than-100000-young-people-in-the-US-live-with-inflammatory-bowel-disease.aspx
- Epidemiologic profile of inflammatory bowel disease in Eastern Mediterranean Region (EMRO) countries: a systematic review and meta-analysis – BMC Public Health – https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-18816-z
- Incidence, Prevalence and Racial and Ethnic Distribution of Inflammatory Bowel Disease in the United States – https://pmc.ncbi.nlm.nih.gov/articles/PMC10592313/
- IBD Facts and Stats – https://www.cdc.gov/inflammatory-bowel-disease/php/facts-stats/index.html
- Epidemiology of Inflammatory Bowel Disease across the Ages in the Era of Advanced Therapies – https://pmc.ncbi.nlm.nih.gov/articles/PMC11522978/
- Dissecting the rising tide of inflammatory bowel disease among youth in a changing world: insights from GBD 2021 – International Journal of Colorectal Disease – https://link.springer.com/article/10.1007/s00384-025-04821-0
- Data mining and analysis of adverse events of Vedolizumab based on the FAERS database – Scientific Reports – https://www.nature.com/articles/s41598-024-75421-1
- Frontiers | Global burden of inflammatory bowel disease in the elderly: trends from 1990 to 2021 and projections to 2051 – https://www.frontiersin.org/journals/aging/articles/10.3389/fragi.2024.1479928/full
- Trends in IBD Incidence, Prevalence, and Biological Therapy – https://www.uspharmacist.com/article/trends-in-ibd-incidence-prevalence-and-biological-therapy
- The national burden of inflammatory bowel disease in the United States from 1990-2019: results from the Global Burden of Disease study database – https://pmc.ncbi.nlm.nih.gov/articles/PMC11226748/
- Rising Incidence of Inflammatory Bowel Disease in the Asian Subcontinent—An Exploration of Causative Factors – https://www.mdpi.com/2624-5647/6/2/38
- Real-World Patterns and Economic Burden Associated With Treatment Failure With Advanced Therapies in Patients With Moderate-to-Severe Ulcerative Colitis – https://pmc.ncbi.nlm.nih.gov/articles/PMC11094759/
- Bridging the gap: Unveiling the crisis of physical inactivity in inflammatory bowel diseases – https://pmc.ncbi.nlm.nih.gov/articles/PMC11000091/
- Frontiers | Association of diet and outdoor time with inflammatory bowel disease: a multicenter case-control study using propensity matching analysis in China – https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2024.1368401/full
- Physical activity in the prevention and management of inflammatory bowel disease: a systematic review – Journal of Public Health – https://link.springer.com/article/10.1007/s10389-024-02278-z
- Recent trends in the epidemiology and clinical outcomes of inflammatory bowel disease in South Korea, 2010-2018 – https://pmc.ncbi.nlm.nih.gov/articles/PMC10989502/
- Recent Advances in the Management of Acute Severe Ulcerative Colitis – https://www.mdpi.com/2077-0383/13/23/7446
- Inequalities in Healthcare Access, Experience and Outcomes in Adults With Inflammatory Bowel Disease: A Scoping Review – https://pmc.ncbi.nlm.nih.gov/articles/PMC11630313/
- Health-care resource use and costs associated with inflammatory bowel disease in northwest London: a retrospective linked database study – BMC Gastroenterology – https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-024-03559-3
- Advances in Inflammatory Bowel Disease Diagnostics: Machine Learning and Genomic Profiling Reveal Key Biomarkers for Early Detection – https://pmc.ncbi.nlm.nih.gov/articles/PMC11172026/
- Frontiers | Advancements in the use of AI in the diagnosis and management of inflammatory bowel disease – https://www.frontiersin.org/journals/robotics-and-ai/articles/10.3389/frobt.2024.1453194/full
- Current Status, Challenges, and Future Directions in Crohn’s Disease – https://pmc.ncbi.nlm.nih.gov/articles/PMC11355312/