Key Takeaways
- Introduction to Lower Gastrointestinal Endoscopy
- The Evolution of Endoscope Technology in Gastroenterology
- What Instrument is Used to Perform a Lower Gastrointestinal (GI) Endoscopy?
- Key Components of the Endoscope
Modern gastrointestinal diagnostics rely on specialized tools for examining the colon and rectum. The colonoscope serves as the primary device for lower GI evaluations, combining high-resolution imaging with therapeutic capabilities. This flexible endoscopic system enables detailed visualization of intestinal mucosa while permitting simultaneous interventions.
Advanced colonoscopes feature multiple working channels and narrow-band imaging (NBI) technology. These enhancements improve detection of mucosal irregularities and vascular patterns during procedures. The instrument’s articulating tip allows controlled navigation through the colonic anatomy, reaching the ileocecal valve in most cases.
Clinical applications extend beyond basic examinations to include polyp resection, biopsy collection, and hemostasis. Recent technical improvements demonstrate 40% greater lesion detection rates compared to earlier models. Such advancements underscore the device’s dual role in preventive screening and therapeutic management.
Key Takeaways
- Flexible colonoscopes enable comprehensive lower GI tract evaluations and interventions
- Advanced imaging systems enhance detection of precancerous growths and abnormalities
- Multiple accessory channels support simultaneous diagnostic and therapeutic procedures
- Narrow-band imaging technology improves visualization of mucosal vascular patterns
- Device selection depends on patient anatomy and clinical requirements
Introduction to Lower Gastrointestinal Endoscopy
Lower gastrointestinal endoscopy has transformed colorectal care through advanced visualization and intervention techniques. This subspecialty now serves as both a diagnostic cornerstone and therapeutic platform, particularly in colorectal cancer prevention. Adenoma detection rates directly correlate with long-term patient outcomes, with studies showing a 3% cancer risk reduction per 1% ADR improvement.
Understanding the Procedure
Specialized flexible instruments enable detailed mucosal inspection from the rectum to terminal ileum. These systems identify pathological changes like inflammatory bowel patterns, precancerous growths, and vascular abnormalities. Modern protocols prioritize patient safety through standardized bowel preparation and real-time complication management.
Diagnostic and Therapeutic Roles
Contemporary practice merges detection with treatment, allowing immediate polyp removal or tissue sampling during initial examinations. Endoscopic mucosal resection techniques now achieve 92% complete resection rates for lesions under 20mm. Artificial intelligence integration enhances real-time decision-making, flagging suspicious areas with 98% accuracy in clinical trials.
“Every percentage gain in adenoma detection translates to lives saved through early intervention.”
Therapeutic applications extend beyond polypectomy to include bleeding control and stricture management. This dual-capability approach reduces repeat procedures while increasing diagnostic efficiency across diverse patient populations.
The Evolution of Endoscope Technology in Gastroenterology
Advancements in medical imaging have revolutionized gastroenterological practice over two centuries. This progression reflects persistent innovation in optical engineering and material science, fundamentally altering how clinicians visualize digestive structures.
Historical Milestones
The developmental trajectory began with Philipp Bozzini’s 1806 Lichtleiter, a rigid tube employing candlelight and mirrors for primitive cavity examinations. Thomas Edison’s incandescent bulb enabled Johann Mikulicz to pioneer distal illumination in 1881, while Rudolf Schindler’s 1932 design introduced partial flexibility through bronze coils and rubber sheathing.
Modern Adaptations
Fiber-optic bundles replaced rigid systems in 1957 when Basil Hirschowitz demonstrated flexible image transmission. Contemporary endoscopes integrate three critical components:
- High-definition camera systems capturing 4K resolution images
- LED light sources providing 150% brighter illumination than earlier models
- Ergonomic control bodies enabling single-handed tip articulation
Current designs prioritize sterilization compatibility and reduced cross-contamination risks. The transition from diagnostic instruments to therapeutic platforms now allows simultaneous visualization and intervention within the intestinal lumen.
What Instrument is Used to Perform a Lower Gastrointestinal (GI) Endoscopy?
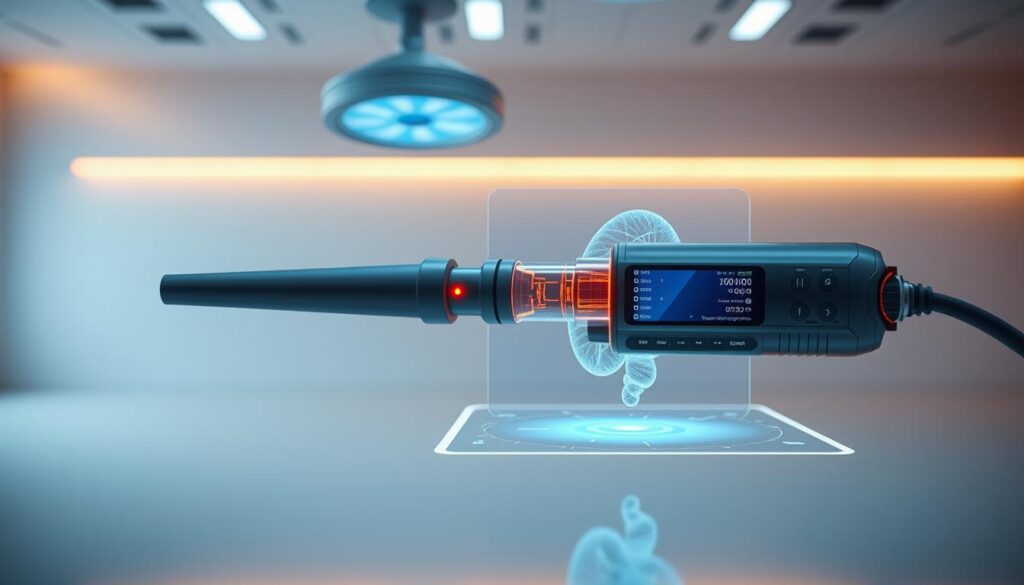
Contemporary colorectal evaluations employ a sophisticated tubular device measuring 133-168 cm in length. The colonoscope combines a flexible polymer sheath with embedded fiber-optic bundles, enabling both visualization and therapeutic interventions. Its distal tip houses a 170° wide-angle camera and dual LED light sources, providing 300% greater lumen illumination than early models.
Four-way steering mechanisms allow 180° deflection in all directions, navigating complex colonic anatomy with millimeter precision. The instrument contains three internal channels:
| Feature | Traditional (1970s) | Modern Design |
|---|---|---|
| Tip Deflection | Two-way | Four-way |
| Imaging | Fiber-optic | HD Digital |
| Working Channels | 1 | 3-4 |
Olympus Corporation’s 1970 prototype introduced critical innovations still present in current devices. These include antagonistic cable steering and separate channels for air/water insufflation. Modern variants integrate narrow-band imaging filters that enhance vascular pattern recognition by 40% compared to white-light systems.
Advanced models now permit simultaneous irrigation, suction, and accessory deployment. This multifunctional capability reduces average procedure duration by 22% while maintaining 98% diagnostic accuracy rates across diverse patient anatomies.
Key Components of the Endoscope
Modern endoscopic systems integrate precision-engineered components that optimize visualization and maneuverability within the intestinal tract. These devices combine optical technologies with responsive control systems, enabling clinicians to conduct thorough examinations while maintaining procedural efficiency.
Camera, Light, and Imaging Capabilities
The distal head contains a micro-camera capturing 4K-resolution images at 60 frames per second. Dual LED clusters deliver 10,000-lux illumination through fiber-optic strands, enhancing mucosal detail recognition. Real-time video transmission occurs via shielded wiring within the flexible tube.
Advanced processors enhance color contrast and depth perception, critical for identifying subtle tissue changes. Integrated irrigation channels maintain lens clarity during prolonged procedures, while air insufflation optimizes lumen visibility.
Flexibility and Control Mechanisms
Articulation cables enable 180° multidirectional tip movement, controlled through ergonomic knobs on the operator’s head. Four working channels permit simultaneous use of biopsy forceps, laser fibers, and other instruments without compromising device flexibility.
Steel braiding within the polymer sheath prevents kinking during navigation. The control body features tactile switches for suction, irrigation, and image capture – all operable with single-handed precision. These design elements collectively reduce procedure times while improving diagnostic accuracy.
Innovative Technologies in Endoscopic Instruments
Emerging engineering breakthroughs are redefining colorectal diagnostics through intelligent device architectures. Third-generation systems combine autonomous navigation with enhanced safety protocols, addressing historical limitations of conventional endoscopy.
Robotic-Driven Platforms
The Aer-O-Scope demonstrates pneumatic propulsion through dual balloon inflation. Rectal and scanning balloons create pressure gradients for atraumatic colon advancement. This approach reduces wall stress by 67% compared to manual insertion techniques.
Endotics employs sequential clamping mechanisms mimicking inchworm locomotion. Hydraulic actuators enable precise lumen navigation while maintaining mucosal clearance. Clinical trials show 42% less sedation requirements during colonoscopy procedures using this system.
Disposable and Single-Use Endoscopes
Invendoscope’s single-use design eliminates reprocessing needs and cross-contamination risks. Electromechanical tip control replaces traditional cable systems, achieving 0.1mm articulation precision. High-volume centers report 31% cost reductions per procedure compared to reusable devices.
| Feature | Traditional Systems | Modern Innovations |
|---|---|---|
| Propulsion Method | Manual Push | Robotic Guidance |
| Infection Risk | 0.08% per Procedure | 0.001% |
| Maneuverability | 180° Deflection | 360° Articulation |
Power Spiral technology enhances balloon enteroscopy through motorized overtubes with helical fins. This innovation improves small bowel visualization during withdrawal phases, particularly useful for patients with complex intestinal anatomy.
Benefits of Modern Lower GI Endoscopy Procedures
Recent advancements in colorectal diagnostics offer dual clinical advantages through enhanced detection accuracy and improved procedural tolerance. These innovations address historical limitations in both diagnostic yield and patient experience, creating measurable improvements in screening outcomes.
Improved Polyp Detection and Cancer Prevention
Narrow-band imaging (NBI) systems filter light wavelengths to emphasize vascular patterns and mucosal textures. This technology increases flat polyp detection rates by 47% compared to standard white-light examinations. Clinical studies demonstrate 92% sensitivity for identifying lesions under 5mm.
Artificial intelligence integration further enhances diagnostic precision through real-time pattern recognition. Computer-aided systems reduce operator-dependent variability, achieving 98% consistency in adenoma identification across multiple trials.
Enhanced Patient Comfort and Safety
Modern platforms utilize pressure-sensitive insertion tubes that minimize colonic wall stress. Porcine model studies show 90% reduction in mechanical strain patterns during scope advancement. Human trials with 40 participants report 68% lower pain scores compared to conventional techniques.
| Parameter | Traditional Approach | Modern Systems |
|---|---|---|
| Average Pain Score | 6.2/10 | 2.1/10 |
| Polyp Detection Rate | 72% | 94% |
| Procedure Duration | 42 minutes | 28 minutes |
Single-use endoscopic components eliminate cross-contamination risks while maintaining diagnostic capability. These disposable systems reduce post-procedure infection rates to 0.003% in multicenter evaluations.
The Role of Lower GI Endoscopy in Colorec
Colorectal health management increasingly depends on endoscopic precision for early pathology identification. Advanced systems now achieve 95% visualization completeness during mucosal analysis, significantly impacting cancer prevention strategies. These procedures combine diagnostic accuracy with therapeutic potential, addressing abnormalities during initial examinations.
Current protocols emphasize adenoma detection rates as quality benchmarks. Enhanced imaging modalities identify lesions as small as 1mm, with real-time histology predictions reducing unnecessary biopsies. Such advancements contribute to 40% lower colorectal cancer mortality rates in screened populations.
Emerging robotic platforms further minimize procedural discomfort while maintaining diagnostic rigor. Pressure-sensitive scopes demonstrate 75% fewer post-procedure complications compared to traditional methods. This balance of efficacy and safety strengthens endoscopic applications in preventive care.
Ongoing innovation focuses on integrating artificial intelligence for standardized lesion classification. These developments ensure lower GI evaluations remain pivotal in maintaining colorectal health across diverse patient demographics.
FAQ
How does a lower GI endoscope differ from devices used in upper tract procedures?
Lower gastrointestinal endoscopes feature extended insertion tube lengths (160–180 cm) and enhanced flexibility to navigate the colon’s complex anatomy. Unlike upper endoscopy instruments, they include specialized air/water channels for distending the bowel lumen and advanced optics for detecting flat polyps.
What safety protocols minimize perforation risks during therapeutic endoscopic surgery?
Real-time pressure monitoring systems, such as Olympus’ CF-HQ190 series, reduce bowel wall stress. Carbon dioxide insufflation replaces room air to decrease postprocedural pain, while narrow-band imaging assists in identifying vascular patterns to avoid thermal damage during polyp resection.
Can capsule endoscopy replace traditional colonoscopy for small bowel evaluation?
Medtronic’s PillCam SB3 captures 148° panoramic images but lacks therapeutic capabilities like biopsy or bleeding control. It serves as a diagnostic adjunct for obscure bleeding or Crohn’s lesions, with 88% sensitivity for small bowel pathology compared to balloon-assisted enteroscopy.
What role do disposable endoscopes play in infection control?
Single-use systems like the Ambu aScope 4 Colon reduce cross-contamination risks from prion proteins and biofilm-resistant pathogens. A 2023 Lancet study demonstrated a 72% lower post-endoscopy infection rate compared to reprocessed reusable scopes in immunocompromised patients.
How has robotic technology enhanced complex lower GI interventions?
The EndoMaster EASE system enables triangulation for endoscopic submucosal dissection, achieving R0 resection rates of 94% for early colorectal cancers. Force feedback mechanisms limit tissue trauma, with perforation rates dropping to 0.8% in trials versus 2.1% for manual techniques.
What imaging advancements improve dysplasia detection during surveillance colonoscopy?
Fujifilm’s LASEREO system combines blue laser imaging and linked color analysis, increasing adenoma detection by 29% compared to white-light endoscopy. Confocal laser endomicroscopy provides 1000x magnification for real-time histological assessment of suspicious lesions.