Key Takeaways
- Understanding ERCP: A Detailed Overview
- Post-ERCP Pancreatitis (PEP): The Most Common Complication
- Risk Factors and Patient Assessment
- How to Manage ERCP Complications
Endoscopic retrograde cholangiopancreatography (ERCP) is a critical diagnostic and therapeutic modality within gastroenterology. Despite its utility, the management of ERCP complications is a pressing concern for healthcare professionals. Post-ERCP pancreatitis (PEP), the most prevalent complication, impacts approximately 10% of patients undergoing this procedure1.
The spectrum of risks associated with ERCP spans from mild discomfort to severe complications. In extreme instances, PEP can precipitate organ failure and mortality. Healthcare providers must possess a deep understanding of these risks to guarantee optimal patient outcomes1.
Recent investigations have revealed a post-ERCP septicemia incidence of 19.1%, underscoring the imperative for effective prevention strategies2. The occurrence of acute post-ERCP pancreatitis was documented in 17.1% of cases, highlighting the significance of meticulous patient selection and risk assessment2.
The intricacy of ERCP procedures is reflected in the diverse definitions of difficult cannulation. The European Society of Gastrointestinal Endoscopy (ESGE) employs the “5-5-1” rule, whereas the American Society for Gastrointestinal Endoscopy (ASGE) emphasizes time and attempt limitations1. These guidelines underscore the necessity for proficient practitioners and sophisticated techniques in ERCP complications management.
Key Takeaways
- Post-ERCP pancreatitis affects about 10% of patients
- Septicemia occurs in 19.1% of ERCP cases
- Acute post-ERCP pancreatitis is seen in 17.1% of procedures
- Proper patient selection and risk assessment are critical
- Advanced techniques and skilled practitioners are essential for managing complications
Understanding ERCP: A Detailed Overview
Endoscopic retrograde cholangiopancreatography (ERCP) emerges as a cornerstone in the realm of gastroenterology, serving as a dual-purpose diagnostic and therapeutic modality for the liver, gallbladder, bile ducts, and pancreas. This ERCP procedure overview elucidates its critical role in contemporary gastroenterological practice3.
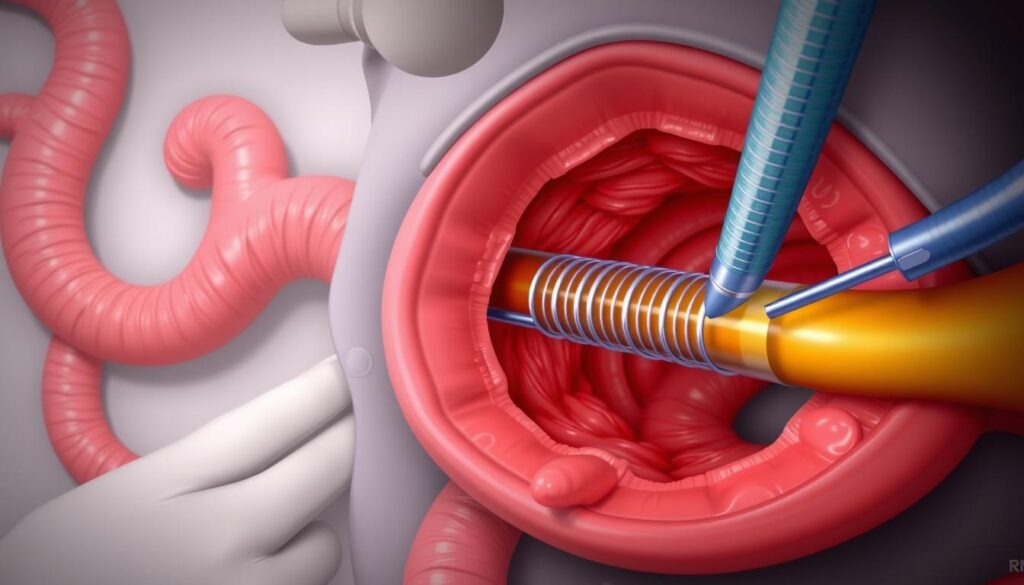
What is ERCP and Its Purpose
ERCP integrates endoscopy and fluoroscopy to facilitate visualization and access to the biliary and pancreatic ducts. It empowers clinicians to diagnose and treat conditions within a single procedural session. The procedure’s primary objective is to address blockages, remove stones, or insert stents into the bile or pancreatic ducts3.
Common Applications in Medical Practice
ERCP indications encompass the treatment of gallstones, the diagnosis and management of pancreatic cancer, and the resolution of bile duct obstructions. It is also employed to investigate unexplained abdominal pain or jaundice. The procedure’s shift from predominantly diagnostic to therapeutic reflects its invasive nature3.
Importance of Proper Patient Selection
The success of ERCP hinges on meticulous patient selection. Factors such as age, medical history, and anatomical considerations are meticulously evaluated. Patients are typically required to fast for several hours prior to the procedure to optimize visualization. Optimal selection mitigates risks like pancreatitis, bleeding, and infection, which, while rare, can occur3.
| ERCP Aspect | Detail |
|---|---|
| Primary Use | Therapeutic interventions |
| Key Benefit | Diagnose and treat in one session |
| Main Risk | Post-ERCP pancreatitis |
| Patient Preparation | Fasting for several hours |
Comprehensive understanding of ERCP’s applications and associated risks is imperative for both healthcare professionals and patients. Such knowledge ensures the judicious application of the procedure, ultimately leading to enhanced patient outcomes in the management of pancreatic and biliary disorders.
Post-ERCP Pancreatitis (PEP): The Most Common Complication
Post-ERCP pancreatitis (PEP) emerges as the quintessential complication ensuing from endoscopic retrograde cholangiopancreatography (ERCP). This affliction impacts up to 15% of patients in the United States, significantly escalating healthcare expenditures and patient morbidity4. Variability in incidence rates is observed globally, with Asian populations experiencing PEP at 10.7% and European populations at 9%5.
Understanding the PEP risk factors is imperative for assessing patient vulnerability. Women and individuals under 50 years old exhibit a heightened susceptibility to this complication4. Those with sphincter of Oddi disorders or a history of acute pancreatitis are also at an elevated risk4. The correlation between the number of cannulation attempts and PEP risk is evident, with rates escalating from 3.3% for fewer than 5 attempts to 14.9% for over 20 attempts5.
The economic toll of PEP is considerable. It contributes approximately $200 million to American healthcare expenses annually, underscoring the imperative for effective prevention and management strategies4. This financial burden, coupled with the risk of severe morbidity and occasional mortality, accentuates the criticality of comprehending and mitigating PEP risks.
| Complication | Incidence Rate | Notable Facts |
|---|---|---|
| Post-ERCP Pancreatitis | 3% – 10% | Most common complication |
| Intra-abdominal Collections | 51.2% | Highest among reported complications |
| Bowel Perforation | 21% | Serious complication requiring immediate attention |
| Hemorrhagic Pancreatitis | 1% – 10% | 50% mortality rate if diagnosis is delayed |
The overall post-ERCP complication rate, based on a systematic survey of 21 prospective clinical studies, is 6.85%6. Acute pancreatitis, the most prevalent complication, exhibits an incidence rate ranging from 3% to 10%6. Grasping these statistics is essential for healthcare providers to effectively manage PEP risk factors and enhance patient outcomes.
Risk Factors and Patient Assessment
ERCP risk assessment necessitates a thorough evaluation of patient-specific factors contributing to complications. This understanding enables healthcare professionals to customize their approach and implement preventive strategies effectively.
Age and Gender Considerations
Age and gender are critical determinants in ERCP outcomes. Women and individuals under 65 years of age exhibit a heightened risk for post-ERCP pancreatitis (PEP)7. A study involving 172 participants revealed a gender distribution of 57% male and 43% female, with a mean age of 53.77 ± 20.20 years8.
Medical History Impact
A patient’s medical history profoundly influences ERCP risks. Individuals with hyperlipidemia or a recent history of acute pancreatitis are at an increased risk for PEP7. Notably, diabetic patients exhibit a lower risk for PEP7. The most prevalent indication for ERCP is common bile duct stone, accounting for 36% of cases8.
Anatomical Challenges
Anatomical variations can complicate ERCP procedures. Complications during ERCP occur in 2.3% of patients, including sphincterotomy perforation (1.2%), hemorrhage (0.6%), and CBD perforation (0.6%)8. Post-ERCP complications affect 2.9% of patients, with retroperitoneal/sphincterotomy perforation being the most common (1.2%)8.
| Complication | Incidence Rate |
|---|---|
| Post-ERCP pancreatitis | 3-10% |
| Cholangitis | 0.5-3% |
| Hemorrhage | 0.3-2% |
| Duodenal perforation | 0.08-0.6% |
ERCP-related complication rates range from 10-12%, with a mortality rate of 0.4-1.4%8. Accurate patient assessment and identification of risk factors are imperative for minimizing these complications.
How to Manage ERCP Complications
Effective ERCP complication management necessitates a multifaceted strategy. The prevalence of benign complications post-ERCP stands at 16.3%, underscoring the imperative for meticulous post-procedure care protocols9. Identifying risk factors and deploying preventive measures are indispensable in curtailing adverse outcomes.
Immediate Response Protocols
Timely identification of complications is critical. The European Society of Gastrointestinal Endoscopy (ESGE) employs the “5-5-1” criterion to delineate “difficult cannulation,” a predictive indicator of procedural risks1. Protocols for immediate response must be established to address post-ERCP pancreatitis, a complication affecting 3-15% of patients1.
Treatment Strategies
Interventional strategies are contingent upon the nature of the complication. For recurrent choledocholithiasis, which manifests in 12.1% of instances, repeat ERCP may be indispensable9. Cholangitis, affecting 4.7% of individuals, necessitates aggressive antibiotic therapy9. Utilizing specialized tools, such as sphincterotomes and guidewires, can facilitate the management of challenging biliary access1.

Monitoring Requirements
Post-ERCP surveillance is critical for the early detection of complications. Patients aged 50 or older, or those with a history of biliary surgery, require intensified monitoring due to heightened risk9. Follow-up care should extend beyond two years, as some complications may manifest later9. Employing wire-guided techniques and transitioning from single to double wire methods in complex scenarios can enhance success rates and diminish adverse event frequencies1.
By rigorously adhering to these ERCP complication management strategies and post-ERCP care protocols, healthcare professionals can markedly enhance patient outcomes and mitigate the likelihood of enduring complications.
Preventive Strategies for Post-ERCP Pancreatitis
Post-ERCP pancreatitis (PEP) impacts up to 15% of patients undergoing endoscopic retrograde cholangiopancreatography in the United States, contributing approximately $200 million to healthcare expenses annually4. With nearly 700,000 ERCP procedures performed yearly in the USA, the imperative to diminish post-ERCP pancreatitis risk is profound10.
PEP prevention techniques pivot on patient risk assessment and targeted interventions. Women, individuals under 50, and those with sphincter of Oddi disorders or a history of acute pancreatitis are at heightened PEP risk4. Endoscopists employ a multi-faceted approach to mitigate these risks.
Rectal nonsteroidal anti-inflammatory drugs (NSAIDs) are a cornerstone of PEP prevention. Their use among gastroenterologists escalated from 62% to 93% between 2013 and 2020, underscoring their efficacy10. Rectal NSAIDs have been shown to reduce pancreatitis risk by approximately 50%11.
Aggressive hydration protocols have gained traction in reducing post-ERCP pancreatitis risk. High-volume intravenous fluid administration can lower overall PEP risk by 50%, though its impact on severe cases remains limited1011.
Pancreatic duct stenting, predominantly for high-risk patients, is another critical strategy. Prophylactic pancreatic ductal stents reduced PEP risk by 65%, marking it as the only intervention proven to decrease severe PEP risk11. Despite its efficacy, pancreatic stents are employed in less than 10% of high-risk patients, indicating a need for enhanced implementation11.
| Prevention Strategy | Risk Reduction | Usage Rate |
|---|---|---|
| Rectal NSAIDs | 50% | 93% of gastroenterologists |
| Aggressive Hydration | 50% (overall) | Data not available |
| Pancreatic Duct Stenting | 65% | <10% in high-risk patients |
By amalgamating these PEP prevention techniques, endoscopists can significantly diminish post-ERCP pancreatitis risk, ameliorating patient outcomes and curtailing healthcare costs associated with this prevalent complication.
Role of Rectal NSAIDs in Complication Prevention
Rectal NSAIDs for ERCP are instrumental in averting post-ERCP pancreatitis (PEP). These anti-inflammatory agents have been proven to significantly diminish the risk of complications. A systematic review encompassing 10 randomized controlled trials with 2006 participants revealed that rectal NSAIDs halved the PEP risk in high-risk cohorts12.
Types of NSAIDs
Several NSAIDs are employed for PEP prevention:
- Indomethacin: Widely studied and recommended
- Diclofenac: Shown efficacy in unselected patients
- Naproxen: Effective in reducing PEP incidence
Diclofenac has emerged as superior in recent meta-analyses, indicating its possible superiority over indomethacin in PEP prevention12.
Timing and Administration
The timing of NSAID administration is critical:
- Administer rectally before or immediately after ERCP
- Standard dose: 100 mg for adults
- Pediatric dose: 10 mg/kg intravenously (for ibuprofen)
Combining rectal NSAIDs with aggressive hydration protocols has shown to further reduce PEP incidence compared to NSAIDs alone13.
Contraindications
While rectal NSAIDs are generally safe, there are contraindications:
- Active peptic ulcer disease
- Severe renal impairment
- Known allergy to NSAIDs
The cost-effectiveness of rectal NSAIDs is notable, with a single dose of 100 mg diclofenac costing approximately $0.1914. This low cost, combined with their efficacy, makes rectal NSAIDs a valuable tool in ERCP complication prevention.
| NSAID | PEP Reduction | Patient Group |
|---|---|---|
| Indomethacin | 54% | Average-risk patients |
| Diclofenac | Significant | Unselected patients |
| Naproxen | 56.5% | High-risk patients |
Aggressive Hydration Protocols
In the realm of ERCP, hydration emerges as a critical factor in mitigating complications. The implementation of aggressive fluid management protocols for PEP prevention has garnered significant attention. Research suggests that such an approach can halve the risk of post-ERCP pancreatitis, albeit with ambiguous implications for severe instances11.
The efficacy of hydration protocols exhibits variability. In the United States, fluid therapy is employed in more than 80% of ERCP procedures among average-risk patients15. The precise timing and volume of fluid administration, though, continue to be the focus of ongoing investigations.
A recent investigation compared the outcomes of high-volume versus standard-volume lactated Ringer’s solution during ERCP. The findings revealed PEP incidence rates of 3% and 11.6% respectively, underscoring the advantages of aggressive hydration16. Notably, another trial reported no discernible difference in PEP rates between intervention and control groups, with rates of 6.7% and 6.3% respectively16.
Despite the promising results, the cost-effectiveness of aggressive hydration remains a topic of debate. The initial strategy necessitated overnight patient stays, which significantly increased healthcare expenditures11. To solidify the efficacy of aggressive hydration in ERCP procedures, further research is imperative. It is essential to establish standardized protocols and elucidate the long-term advantages of this approach.
Pancreatic Stent Placement Guidelines
The deployment of pancreatic stents during ERCP emerges as a vital strategy for mitigating post-ERCP pancreatitis (PEP). This intervention necessitates meticulous patient selection and the possession of advanced technical acumen to optimize its efficacy.
Patient Selection Criteria
Accurately identifying patients at heightened risk for complications is fundamental to the consideration of pancreatic stent placement in ERCP. Indicators such as suspected sphincter of Oddi dysfunction and the challenge of cannulation are deemed critical17. Data indicate that approximately 26-27% of patients are suspected to have sphincter of Oddi dysfunction, with 82-84% experiencing difficulties in cannulation17.
Technical Considerations
The success of stent placement hinges on its precise execution. Notably, up to 20% of patients assigned to prophylactic pancreatic ductal stent placement may experience failure17. This underlines the imperative for endoscopists to possess advanced skills and undergo rigorous training in stent deployment methodologies.
Post-placement Care
Post-stent deployment, patients necessitate vigilant monitoring. Regular follow-up assessments and diagnostic imaging are indispensable for ensuring the stent’s optimal positioning and functionality18. Patients must adhere to a regimen of adequate hydration and a nutritionally balanced diet to facilitate stent efficacy and avert complications18.
Despite the existence of well-defined prophylactic stenting protocols, their implementation remains suboptimal. A study revealed that 16% of patients with common bile duct stones underwent stent insertion not in accordance with guidelines19. Yet, targeted quality improvement initiatives can significantly diminish unnecessary stent placements, leading to fiscal benefits and enhanced patient well-being19.
Pancreatic stent placement stands as a critical tool in the management of ERCP-related complications. Adherence to established guidelines and the enhancement of implementation rates can significantly elevate patient care standards and diminish the incidence of post-ERCP pancreatitis.
Managing Infectious Complications
Infectious complications in ERCP procedures are a significant concern. A study of 32,972 ERCP hospitalizations revealed that 19.1% of patients developed post-ERCP septicemia, with 6.9% experiencing acute cholangitis2. These findings underscore the critical need for effective prevention and management strategies for ERCP-related infections.
Prevention Strategies
Preventing ERCP-related infections involves several key approaches:
- Proper sterilization of equipment
- Aseptic procedural practices
- Antibiotic prophylaxis in high-risk cases
Research indicates that antibiotic prophylaxis may reduce the risk of septicemia, with an adjusted odds ratio of 0.85 for patients receiving preventive antibiotics2. Its effectiveness, though, varies across different complications.
Treatment Approaches
When ERCP-related infections occur, prompt and targeted treatment is critical. Cholangitis management post-ERCP typically involves:
- Early recognition of symptoms
- Microbiological cultures to identify pathogens
- Targeted antibiotic therapy
- Biliary drainage if necessary
In liver transplant patients, who are at higher risk for infectious complications, the median hospitalization duration after ERCP was 4 days20. This highlights the importance of close monitoring and aggressive treatment in high-risk groups.
By implementing robust prevention strategies and timely treatment approaches, healthcare providers can significantly reduce the incidence and impact of ERCP-related infections. This improves patient outcomes and reduces healthcare costs.
Training and Technical Expertise Requirements
ERCP training necessitates a profound level of proficiency in complication management, a critical aspect for gastroenterology fellows. The acquisition of such expertise demands extensive practice, as evidenced by a study indicating that even those with over 200 upper endoscopic procedures require dedicated ERCP training21.
The learning curve for ERCP is formidable. Trainees in the study were required to perform each key procedure – duodenoscope insertion, biliary cannulation, and plastic stent insertion – five times. The results were impressive, with success rates reaching 94% for duodenoscope insertion, 100% for biliary cannulation, and 92% for plastic stent insertion21.
Mastering the management of ERCP complications is imperative. The incidence of pancreatitis as an ERCP-related adverse event ranges from 3% to 15%. Difficult biliary access, occurring in 5% to 10% of cases, necessitates additional training and can significantly prolong procedural time by 30% to 50%22.
Continuous education remains essential. Training programs focused on advanced ERCP techniques report a 25% increase in procedural success rates. Without specialized training, success rates for complex cases may plummet below 50%22.
| Procedure | Success Rate | Mean Satisfaction Score |
|---|---|---|
| Duodenoscope Insertion | 94% | 4.4/5 |
| Biliary Cannulation | 100% | 4.7/5 |
| Plastic Stent Insertion | 92% | 4.6/5 |
ERCP expertise is of particular importance in specific patient populations. For instance, in patients who have undergone Roux-en-Y gastric bypass (RYGB), ERCP is frequently required for biliary stones, which occur in 47% of cases23. This highlights the necessity for endoscopists to possess the skills to perform ERCP in altered anatomy.
Cost Considerations and Healthcare Impact
ERCP complication costs exert a considerable strain on healthcare systems. It is imperative to grasp the financial implications and the healthcare economics of endoscopic procedures. This understanding is vital for effective management and resource allocation.
Financial Implications
Post-ERCP pancreatitis (PEP) incurs an additional $200 million annually in American healthcare expenses. This substantial financial burden highlights the necessity for effective prevention strategies. The escalating cost of rectal indomethacin, a common preventive measure, has prompted the exploration of alternative NSAID formulations to enhance cost-effectiveness.
Insurance Coverage
Insurance policies exhibit variability in their coverage of ERCP complications. Some plans may not fully cover preventive measures, resulting in out-of-pocket expenses for patients. Healthcare providers must navigate these complexities to ensure optimal patient care while managing costs.
Healthcare System Impact
ERCP complications strain healthcare resources, impacting patient care quality and system efficiency. The British Society of Gastroenterology’s ERCP endoscopy quality improvement project (EQIP) established 70 consensus statements to enhance service delivery. These statements address aspects from patient booking to follow-up24. This initiative reflects the growing focus on improving ERCP outcomes and reducing system-wide impacts.
| Aspect | Recommendation |
|---|---|
| Treatment Timeframe | Patients with CBD stones and jaundice should be treated within 72 hours of diagnosis24 |
| Recovery Period | Minimum 4 hours, with 2 hours sufficient in select cases24 |
| Complication Management | ERCP units must have policies for prevention and recognition of complications24 |
These guidelines aim to standardize care, potentially reducing complications and associated costs. By implementing such measures, healthcare systems can work towards minimizing the economic impact of ERCP complications while improving patient outcomes.
Conclusion
The management of ERCP complications stands as a cornerstone in gastroenterology patient care. A review of 32,972 ERCP procedures for Primary Sclerosing Cholangitis revealed that 39.1% of patients received antibiotic prophylaxis, underscoring the ongoing debate on preventive measures2. The significance of adhering to ERCP best practices is highlighted by the risk of severe complications, as exemplified by a case of life-threatening air embolism during the procedure25.
Advancements in endoscopic procedure safety have led to improved outcomes, yet challenges persist. A study of 603 ERCP procedures found that 27.9% resulted in irretrievable stones, necessitating alternative approaches26. This data reinforces the imperative for personalized risk assessment and tailored strategies to elevate ERCP success rates and mitigate complications.
The trajectory forward necessitates the refinement of ERCP techniques and an expanded comprehension of risk factors. The field continues to evolve, with research indicating varying success rates between repeat ERCP (86.0%) and common bile duct exploration (92.1%) for challenging cases26. By prioritizing patient safety, fostering ongoing education, and adhering to best practices, we can strive to diminish the occurrence of complications such as post-ERCP pancreatitis, which affected 17.1% of patients in a large-scale study2. The concerted efforts of healthcare providers, researchers, and policymakers are essential in propelling ERCP safety and efficacy, ultimately leading to enhanced patient outcomes in gastroenterology.
FAQ
What is ERCP and why is it performed?
ERCP, or Endoscopic Retrograde Cholangiopancreatography, integrates endoscopy and fluoroscopy to diagnose and treat disorders affecting the pancreatic and biliary tracts. Primarily, it serves a therapeutic purpose, including gallstone removal, stent placement, and treatment of strictures in the bile or pancreatic ducts.
What is the most common complication of ERCP?
The prevalent complication of ERCP is post-ERCP pancreatitis (PEP). This condition can vary from mild to severe, leading to considerable morbidity and increased healthcare expenditures if not effectively managed.
What are the main risk factors for ERCP complications?
ERCP complications are influenced by patient-specific factors such as age, gender, and medical history, alongside anatomical challenges that elevate procedural difficulty. Specific risk factors for PEP include female gender, younger age, recurrent pancreatitis history, and challenging pancreatic duct cannulation.
How can post-ERCP pancreatitis be prevented?
Preventing post-ERCP pancreatitis involves a multifaceted approach. This includes the administration of rectal NSAIDs, aggressive hydration protocols, and pancreatic stent placement in high-risk patients. These preventive measures must be tailored to individual patient risk factors and procedural complexity.
What is the role of rectal NSAIDs in preventing ERCP complications?
Rectal NSAIDs, such as indomethacin or diclofenac, are critical in preventing post-ERCP pancreatitis. They reduce inflammation and are administered immediately before or after the procedure. Their use is recommended due to their cost-effectiveness and favorable safety profile.
How important is hydration in managing ERCP complications?
Hydration protocols are deemed essential in preventing and managing ERCP complications, with a focus on post-ERCP pancreatitis. Intravenous fluids are administered before, during, and after the procedure. The optimal implementation and cost-effectiveness of these protocols are subjects of ongoing research.
When should pancreatic stent placement be considered during ERCP?
Pancreatic stent placement is indicated for patients at high risk of post-ERCP pancreatitis. This includes those with difficult cannulation, pancreatic sphincterotomy, or recurrent pancreatitis history. The decision should be based on individual patient factors and the endoscopist’s expertise in stent placement.
How are infectious complications of ERCP managed?
Infectious complications, such as cholangitis, are managed through prevention strategies like proper sterilization and antibiotic prophylaxis. Prompt recognition and intervention are critical if infection occurs. Treatment involves targeted antibiotic therapy based on microbiological cultures and may require additional interventions for adequate biliary drainage.
What training is required to perform ERCP and manage its complications?
ERCP and its complications require specialized training beyond basic endoscopy skills. Achieving competency involves hundreds of procedures. Ongoing education, skill maintenance, and experience in advanced techniques like pancreatic stent placement are essential. Simulation-based training and proctoring are also vital in developing ERCP expertise.
What are the cost implications of ERCP complications?
ERCP complications can significantly impact costs, including direct expenses from extended hospital stays and additional treatments, as well as indirect costs such as legal liabilities. The economic burden extends to healthcare systems through increased resource utilization. Investing in prevention strategies can lead to long-term cost savings by reducing complication rates and improving patient outcomes.
Source Links
- ERCP Biliary Access – https://www.bostonscientific.com/en-US/medical-specialties/gastroenterology/procedures-and-treatments/ercp-biliary-access.html
- Preventive Antibiotic Use and Complications After Endoscopic Retrograde Cholangiopancreatography in Patients Hospitalized for Primary Sclerosing Cholangitis – https://pmc.ncbi.nlm.nih.gov/articles/PMC11317107/
- ERCP (Endoscopic Retrograde Cholangiopancreatography): All You Need to Know | Omar Rashid, Medicus Elite – https://www.toplinemd.com/omar-rashid/ercp-endoscopic-retrograde-cholangiopancreatography-all-you-need-to-know/
- Preventing Pancreatitis After ERCP – https://www.hopkinsmedicine.org/news/articles/2024/03/preventing-pancreatitis-after-ercp
- Post-endoscopic Retrograde Cholangiopancreatography Hemorrhagic Pancreatitis in a Young Female: A Case Report – https://pmc.ncbi.nlm.nih.gov/articles/PMC11193661/
- A Study on the Spectrum of Imaging Findings of Post-ERCP-Specific Complications: A Retrospective Descriptive Study – https://pmc.ncbi.nlm.nih.gov/articles/PMC11188732/
- Risk factors for and Strategies to Prevent Complications of Endoscopic Retrograde Cholangiopancreatography – https://www.diva-portal.org/smash/get/diva2:1567035/FULLTEXT01.pdf
- Predicting acute complications in endoscopic retrograde cholangiopancreatography based on the severity and onset of post-procedural pain – Egyptian Liver Journal – https://eglj.springeropen.com/articles/10.1186/s43066-024-00355-2
- PDF – https://www.eajm.org/Content/files/sayilar/229/1-6.pdf
- A Systematic Review and Individual Patient Data Meta-Analysis – https://www.pancreoscopieonline.com/mpl/pb.mpl?x=fa36d1f5b9c9d76316dc2c95428c7ea6801a53cb042bd6efaeae94b1add201f767816bec66ddd01a2705b9eda1973abdf8fb1cfb1a96def7dad67c9212781d3e901d024a0990f9ae5a1a4d2e2562de540593ef3e5d9704e9
- ASGE Guidelines Give Practical Advice to Prevent Most Common Complication of ERCP – DDW News – https://news.ddw.org/news/asge-guidelines-give-practical-advice-to-prevent-most-common-complication-of-ercp/
- Nonsteroidal Anti-inflammatory Drugs for the Prevention of Post-endoscopic Retrograde Cholangiopancreatography Pancreatitis – https://pmc.ncbi.nlm.nih.gov/articles/PMC11415478/
- Efficacy of hydration combined with rectal non-steroidal anti-inflammatory drugs (NSAIDs) versus NSAIDs alone for the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis: A systematic review and meta-analysis – https://www.researchsquare.com/article/rs-5359932/v1.pdf?c=1733197594000
- Nonsteroidal anti-inflammatory drugs before endoscopic ultrasound guided tissue acquisition to reduce the incidence of post procedural pancreatitis – https://pmc.ncbi.nlm.nih.gov/articles/PMC10950633/
- Aggressive hydration with lactated Ringer’s solution versus plasma solution for the prevention of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis (ALPS study): protocol for a multicentre, double-blind, randomised controlled trial – https://pmc.ncbi.nlm.nih.gov/articles/PMC11218011/
- High-volume lactated Ringer’s solution with human albumin versus standard-volume infusion as a prophylactic treatment for post-endoscopic retrograde cholangiopancreatography pancreatitis: randomized clinical trial – https://pmc.ncbi.nlm.nih.gov/articles/PMC11749547/
- Add Pancreatic Duct Stent to Indomethacin to Minimize Post-ERCP Pancreatitis in High-Risk Patients – American College of Gastroenterology – https://gi.org/journals-publications/ebgi/schoenfeld1_feb2024/
- The Impact of ERCP Stent on Your Health | Unio Specialty Care – https://uniospecialtycare.com/resources/the-impact-of-ercp-stent-on-your-health/
- Optimising the indications for biliary stent placement during endoscopic retrograde cholangiopancreatography: a quality improvement initiative to enhance patient care and reduce healthcare resource utilisation – https://pmc.ncbi.nlm.nih.gov/articles/PMC11340697/
- Risk Factors for Infectious Complications following Endoscopic Retrograde Cholangiopancreatography in Liver Transplant Patients: A Single-Center Study – https://www.mdpi.com/2077-0383/13/5/1438
- Endoscopic retrograde cholangiopancreatography training using a silicone simulator fabricated using a 3D printing technique (with videos) – Scientific Reports – https://www.nature.com/articles/s41598-025-86755-9
- Management of difficult biliary access during ERCP in adults – https://www.uptodate.com/contents/management-of-difficult-biliary-access-during-ercp-in-adults
- Laparoscopic-assisted transgastric endoscopic retrograde cholangiopancreatography: a review of indications, technical considerations, and outcomes – https://ales.amegroups.org/article/view/10014/html
- British Society of Gastroenterology Endoscopic Retrograde Cholangiopancreatography (ERCP) Quality Improvement Programme: minimum service standards and good practice statements – https://fg.bmj.com/content/15/6/445
- Systemic air embolism associated with endoscopic retrograde cholangiopancreatography: A case report – https://www.wjgnet.com/1948-5190/full/v16/i11/617.htm
- Repeat ERCP versus Common Bile Duct Exploration for Failed Stone Clearance: A Prospective Randomized Study – https://www.clinmedjournals.org/articles/ijsrp/international-journal-of-surgery-research-and-practice-ijsrp-11-171.php?jid=ijsrp