Key Takeaways
- Understanding IBD: Overview and Clinical Significance
- The Role of Laboratory Testing in IBD Diagnosis
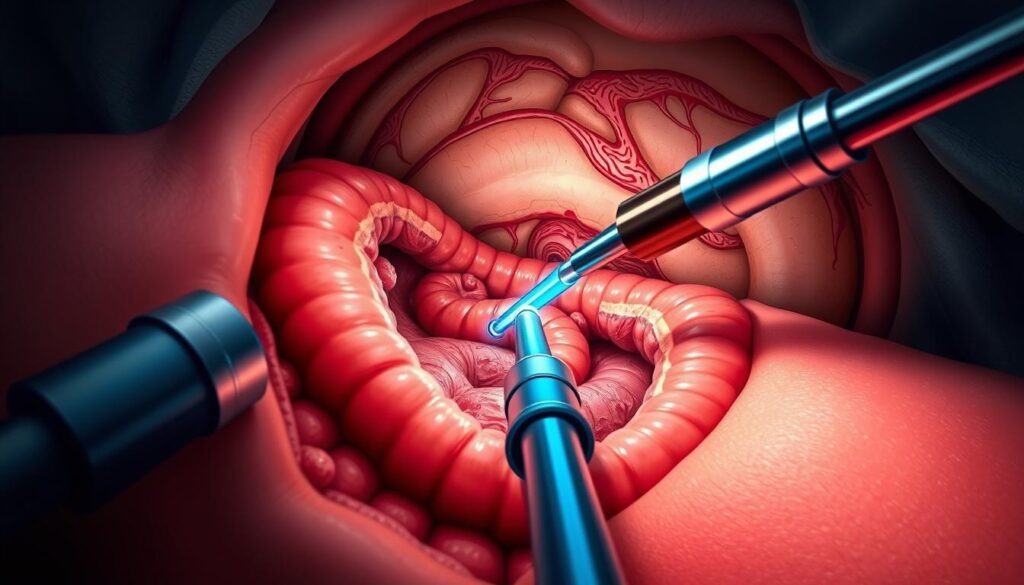
- Endoscopy in Inflammatory Bowel Disease (IBD)
- Advanced Endoscopic Techniques for IBD Assessment
Inflammatory Bowel Disease (IBD) presents formidable challenges to gastrointestinal health. This guide delves into the indispensable role of endoscopy in diagnosing and managing IBD. The global prevalence of IBD has escalated, with patient numbers escalating from 3.3 million in 1990 to 4.9 million in 20191. Endoscopic procedures are indispensable for evaluating gastrointestinal inflammation and distinguishing between ulcerative colitis and Crohn’s disease.
The impact of IBD on quality of life is considerable. With appropriate medical intervention, most patients can experience symptom-free periods lasting one to three years2. Routine colonoscopies are imperative for IBD patients due to the heightened risk of colorectal cancer associated with chronic colon inflammation2. This guide seeks to augment medical professionals’ comprehension of endoscopic techniques in IBD care.
Diagnostic tools for IBD encompass blood tests to detect infections, anemia, and inflammation markers. Stool samples aid in identifying blood, organisms, or inflammatory markers such as calprotectin2. Colonoscopy stands as the gold standard, providing a thorough examination of the colon and segments of the small intestine, frequently accompanied by biopsies to differentiate IBD from other inflammatory conditions2.
Key Takeaways
- Global IBD prevalence has increased significantly from 1990
- Endoscopy plays a critical role in IBD diagnosis and management
- Regular colonoscopies are vital for colorectal cancer screening in IBD patients
- Blood tests and stool samples are key diagnostic tools
- Colonoscopy with biopsy is the primary method for IBD diagnosis
- Various endoscopic procedures cater to different diagnostic needs in IBD
Understanding IBD: Overview and Clinical Significance
Inflammatory Bowel Disease (IBD) encompasses chronic conditions characterized by gastrointestinal inflammation. The two primary forms of IBD are ulcerative colitis and Crohn’s disease. These disorders result from a complex interplay of genetic factors, environmental triggers, and immune system dysfunction.
Types of Inflammatory Bowel Disease
Ulcerative colitis predominantly affects the colon’s mucosal layer, whereas Crohn’s disease can impact any part of the digestive tract, causing transmural inflammation. Endoscopic scoring systems are critical for assessing mucosal healing in both conditions3.
Disease Burden and Global Prevalence
IBD epidemiology reveals a growing global prevalence, posing significant challenges to healthcare systems worldwide. The complexity of current scoring systems highlights the need for improved training and resources for gastroenterologists3.
Clinical Manifestations and Complications
IBD presents with diverse symptoms, ranging from abdominal pain to extraintestinal manifestations. Complications can include strictures, fistulas, and an increased risk of colorectal cancer. Endoscopy plays a vital role in evaluating disease activity, treatment response, and predicting patient outcomes3.
| Condition | Primary Location | Endoscopic Scoring System |
|---|---|---|
| Ulcerative Colitis | Colon (Mucosal Layer) | Mayo Endoscopic Score (MES), Ulcerative Colitis Endoscopic Index of Severity (UCEIS) |
| Crohn’s Disease | Entire Digestive Tract | Crohn’s Disease Endoscopic Index of Severity (CDEIS), Simple Endoscopic Score for CD (SES-CD) |
Recent advancements in endoscopic techniques, such as virtual chromoendoscopy, enhance visualization and improve differentiation between remission and mild disease. Artificial Intelligence shows promise in improving accuracy and consistency in endoscopic scoring3.
The Role of Laboratory Testing in IBD Diagnosis
Laboratory tests are indispensable in the diagnosis and monitoring of Inflammatory Bowel Disease (IBD). They enable clinicians to distinguish between IBD subtypes and gauge disease activity4.
Serological Markers and Blood Tests
Blood tests are fundamental in IBD diagnosis. C-reactive protein (CRP) serves as a critical inflammatory marker, used to assess disease activity. Elevated CRP levels signify active inflammation in IBD patients5.
Antibody tests, such as ANCA and ASCA, are instrumental in distinguishing between ulcerative colitis and Crohn’s disease. ASCA antibodies were detected in 50% of celiac disease patients, underscoring the necessity for meticulous interpretation4.
Stool Studies and Inflammatory Markers
Fecal calprotectin is a significant stool test for IBD diagnosis. It aids in distinguishing IBD from functional gastrointestinal disorders. Notwithstanding its utility, stool tests are insufficient without colonoscopic evaluation5.
Genetic Testing and Biomarkers
Genetic studies have identified over 200 susceptibility loci for IBD, with considerable overlap between Crohn’s disease and ulcerative colitis. These loci account for approximately 13% of disease liability variation4.
Emerging biomarkers hold promise. Serum pyruvate kinase M2 (PKM2) levels were found to be six times higher in IBD patients than in healthy controls. This discovery may pave the way for novel diagnostic tools4.
While laboratory tests are invaluable, their efficacy is maximized when integrated with clinical assessment and endoscopic evaluation for precise IBD diagnosis and management.
Endoscopy in Inflammatory Bowel Disease (IBD)
Endoscopy is indispensable in the diagnosis and management of inflammatory bowel disease (IBD). This discourse delves into the array of endoscopic methodologies, their distinct characteristics, and the biopsy protocols for IBD evaluation.
Types of Endoscopic Procedures
Varied endoscopic modalities are employed to assess IBD. Colonoscopy enables the examination of the entire colon and segments of the small intestine. In contrast, flexible sigmoidoscopy focuses on the lower colon and rectum. Capsule endoscopy offers visualizations of the small intestine. These methods are instrumental in diagnosing IBD, determining its extent, and evaluating treatment efficacy67.
Endoscopic Features of IBD
Gastroenterologists during endoscopy seek out specific IBD endoscopic markers. These include mucosal inflammation, ulcers, and pseudopolyps. Ulcerative colitis is characterized by continuous inflammation of the colon lining. In contrast, Crohn’s disease exhibits patchy inflammation and skip lesions. These visual indicators are critical in distinguishing between IBD subtypes and assessing their severity.
Biopsy Sampling Guidelines
Biopsy sampling during endoscopy is vital for confirming IBD diagnosis. Tissue samples are obtained from both inflamed and unaffected areas. For suspected ulcerative colitis, biopsies are taken from the rectum and various colon segments. In cases of Crohn’s disease, samples may include the terminal ileum. Accurate histological assessment through proper biopsy technique is essential for guiding treatment decisions.
| Endoscopic Procedure | Primary Use in IBD |
|---|---|
| Colonoscopy | Evaluate entire colon, diagnose IBD |
| Sigmoidoscopy | Assess lower colon and rectum |
| Capsule endoscopy | Visualize small intestine |
Endoscopy remains a fundamental tool in IBD management, facilitating diagnosis, treatment monitoring, and cancer surveillance. Ongoing research and the development of novel endoscopic technologies continue to refine our understanding and care of IBD patients8.
Advanced Endoscopic Techniques for IBD Assessment
Endoscopic methodologies have undergone significant evolution, enabling more precise visualization and assessment of inflammatory bowel disease (IBD). At the vanguard of these advancements are chromoendoscopy, narrow-band imaging, and confocal laser endomicroscopy. These innovations seek to elevate the current therapeutic efficacy, which stands at approximately 30% for achieving long-term remission in IBD9.
Chromoendoscopy employs dyes to accentuate mucosal alterations, facilitating the identification of dysplasia. This approach is predominantly geared towards detecting cancerous lesions, as opposed to evaluating IBD activity9. Narrow-band imaging, a virtual chromoendoscopy variant, augments mucosal and vascular contrast without the necessity for dye application9.
Confocal laser endomicroscopy enables real-time histological examination of intestinal mucosa. This technology empowers targeted biopsies and the implementation of personalized medicine strategies in IBD management. The disparity between endoscopic and histological activity severity assessments remains considerable, with a kappa value of 0.4, underscoring the imperative for these advanced methodologies10.
Emerging technologies, such as artificial intelligence-assisted endoscopy, hold promise in augmenting diagnostic precision and streamlining IBD surveillance protocols. These innovations aim to standardize assessments, enhance accuracy, and diminish subjectivity in interpreting endoscopic findings10.
A recent investigation involving 193 gastroenterologists from 12 provincial-level regions in China demonstrated that IBD subspecialists and those with prior training exhibited a greater propensity to employ endoscopic indices (p 3.
Imaging Technologies in IBD Diagnosis
Advanced imaging techniques are indispensable in the diagnosis and management of Inflammatory Bowel Disease (IBD). Cross-sectional imaging methods provide detailed views of the gastrointestinal tract, enabling accurate assessment of bowel wall thickening and extraintestinal complications.
CT Enterography
CT enterography, a specialized form of computed tomography, offers enhanced visualization of the small intestine. It has largely replaced traditional barium X-rays in many medical centers due to its superior ability to detect both mural and extramural disease manifestations. CT enterography excels in spatial resolution, making it valuable for identifying bowel wall thickening and assessing extraintestinal complications.

MR Enterography
MR enterography utilizes magnetic resonance imaging to evaluate the small bowel without exposing patients to ionizing radiation. This method is highly beneficial for assessing fistulas in the perianal region and small intestine. The superior soft tissue contrast of MRI makes it an excellent tool for detecting subtle changes in bowel wall structure and identifying extraintestinal complications associated with IBD.
Ultrasound Applications
Intestinal ultrasound is gaining prominence in IBD management due to its real-time assessment capabilities. This non-invasive technique allows for quick evaluation of bowel wall thickness and vascularity. Ultrasound is highly effective in detecting complications such as strictures and abscesses, providing valuable information for treatment planning.
| Imaging Modality | Key Advantages | Primary Applications |
|---|---|---|
| CT Enterography | High spatial resolution | Mural and extramural disease detection |
| MR Enterography | No radiation, superior soft tissue contrast | Perianal fistulas, small bowel assessment |
| Intestinal Ultrasound | Real-time, non-invasive | Bowel wall thickness, complication detection |
The integration of artificial intelligence (AI) in these imaging technologies is showing promise in improving diagnostic accuracy and reducing variability in image interpretation. AI-assisted endoscopic procedures are linked to increased personalized treatment options, potentially leading to better patient outcomes in IBD care11. Recent studies have demonstrated that AI can achieve high sensitivity in detecting mucosal inflammation through MRI data analysis and has been effective in classifying IBD disease severity12.
Surveillance and Monitoring Strategies
Effective surveillance and monitoring are indispensable for the management of Inflammatory Bowel Disease (IBD). These methodologies are designed to identify complications at their inception and to gauge disease activity, ensuring the delivery of superior patient care.
Cancer Screening Protocols
Individuals with IBD are at a heightened risk of developing colorectal cancer (CRC), with a two- to three-fold increased likelihood compared to the general populace13. This risk intensifies with time, reaching approximately 18% after 30 years of disease duration13. To mitigate this, the implementation of regular colonoscopic surveillance is imperative.
Advanced endoscopic methodologies hold a critical role in the detection of dysplasia. Chromoendoscopy has been shown to surpass standard methods in identifying neoplastic lesions14. High-definition white-light endoscopy (HD-WLE) and dye-based chromoendoscopy (DCE) have demonstrated comparable detection rates of around 18%13.
Follow-up Intervals
CRC surveillance typically commences 8 years post-symptom onset in ulcerative colitis patients with rectal involvement or Crohn’s disease affecting at least one-third of the colon13. High-risk patients necessitate colonoscopies every 1-3 years, whereas low-risk individuals may extend intervals up to 5 years13.
Disease Activity Assessment
Regular evaluation of disease activity is fundamental for the effective management of IBD. Endoscopic scoring systems, such as the Mayo Endoscopic Score for ulcerative colitis, facilitate the assessment of mucosal healing and guide therapeutic decisions. Fecal calprotectin exhibits a high correlation with mucosal inflammation levels and possesses a high negative predictive value for IBD15.
Through the implementation of these surveillance and monitoring strategies, healthcare providers can enhance IBD management, detect complications early, and strive towards achieving endoscopic remission in patients.
Therapeutic Applications of Endoscopy in IBD
Endoscopy emerges as a cornerstone in the management of Inflammatory Bowel Disease (IBD). Notably, endoscopic balloon dilation (EBD) emerges as a preeminent method for addressing strictures in Crohn’s disease. This intervention demonstrates a technical success rate exceeding 90% for short intestinal strictures16.
Research substantiates EBD’s efficacy in treating both anastomotic and de novo strictures. A systematic review encompassing 33 studies reported a 89.1% technical success rate and 80.9% clinical efficacy in 1463 Crohn’s disease patients16. The length of the stricture significantly influences outcomes, with strictures under 5 cm correlating with extended intervals without surgical intervention.
Endoscopic mucosal resection (EMR) also holds a significant place in IBD management. A meta-analysis of 12 studies, encompassing 291 dysplastic lesions in 274 patients, revealed compelling results. The pooled en-bloc resection rate was 92.5%, with an R0 resection rate of 81.5%17.
Despite the benefits these procedures offer, they are not devoid of risks. EBD is associated with a 2.8% per-procedure complication rate16. For EMR, the rates of bleeding and perforation were 7.7% and 5.3% respectively17. The meticulous selection of patients and the application of precise techniques are imperative for achieving optimal results.
| Procedure | Success Rate | Complication Rate |
|---|---|---|
| Endoscopic Balloon Dilation | 89.1% | 2.8% |
| Endoscopic Mucosal Resection | 92.5% | 13% (combined bleeding and perforation) |
These endoscopic modalities present valuable alternatives to surgical interventions in IBD management. They facilitate effective stricture management and dysplasia treatment, significantly improving patient outcomes and quality of life. Ongoing research aims to further refine these methodologies, aiming to enhance their safety and efficacy in the realm of IBD care.
Complications and Safety Considerations
Endoscopic procedures in Inflammatory Bowel Disease (IBD) necessitate meticulous attention to inherent risks and safety protocols. Grasping these nuances is imperative for healthcare professionals and patients alike, aiming for superior outcomes and the reduction of adverse occurrences.
Procedure-Related Risks
Endoscopic interventions in IBD harbor inherent perils, with perforation risk standing as a foremost concern. The likelihood of perforation during colonoscopy escalates in patients with severe inflammation or strictures. Capsule endoscopy is contraindicated in cases of suspected bowel obstruction, as it may precipitate capsule retention. Sedation-related adverse events are prevalent, predominantly in patients with comorbidities or advanced age18.
Patient Preparation Guidelines
Imperative to the success and safety of endoscopic procedures is the meticulous preparation of the patient. This encompasses:
- Thorough bowel cleansing
- Medication adjustments, specially for anticoagulants
- Fasting guidelines
- Detailed medical history review
Patients must be apprised of the procedure and its attendant risks to facilitate informed consent.
Post-Procedure Care
Post-procedure vigilance is critical for the early detection and management of complications. Post-polypectomy bleeding is a notable concern, necessitating vigilant observation. Patients must be monitored for signs indicative of perforation, such as abdominal pain or fever. Explicit discharge instructions, including the parameters for seeking medical attention, should be communicated to all patients19.
By rigorously adhering to these safety protocols and preparation guidelines, healthcare providers can mitigate the risks associated with endoscopic procedures in IBD patients, ultimately ensuring enhanced outcomes and patient contentment.
Conclusion
Endoscopy has evolved into a fundamental pillar in the management of Inflammatory Bowel Disease (IBD), transforming diagnostic, monitoring, and therapeutic paradigms. The incidence of IBD has surged by 46% in Europe over the past two decades, impacting approximately 0.2% of the populace, or 2.5–3 million individuals20. This escalating trend accentuates the imperative for sophisticated endoscopic methodologies in IBD treatment.
Personalized endoscopic methodologies are redefining the trajectory of IBD management. These customized approaches account for individual patient attributes and disease manifestations, facilitating more targeted interventions. For example, fecal calprotectin levels exceeding 250 µg/g signify an 8% probability of IBD development within a year, aiding clinicians in determining the necessity for endoscopic surveillance20. Such individualized care is indispensable, given that up to 20% of Crohn’s disease patients exhibit complications such as strictures or fistulas at diagnosis20.
Looking forward, advancements in IBD management are anticipated to integrate artificial intelligence-assisted endoscopy and molecular imaging. These innovations are expected to elevate diagnostic precision and therapeutic effectiveness. Currently, the overall sensitivity of fecal calprotectin in detecting IBD stands at 85.8%, with a specificity of 91.7%20. Future endeavors in endoscopic techniques aim to refine these metrics, potentially diminishing the 10–15% of IBD cases that remain indeterminate20. As we progress, the confluence of advanced endoscopic technologies and personalized medicine methodologies will be instrumental in optimizing outcomes for IBD patients.
FAQ
What is the primary role of endoscopy in IBD management?
Endoscopy is indispensable in the diagnosis, management, and surveillance of Inflammatory Bowel Disease (IBD). It enables direct visualization of the gastrointestinal mucosa, allowing for the assessment of disease extent and severity. This is complemented by biopsy sampling for histopathological analysis. Endoscopic procedures are vital for distinguishing between ulcerative colitis and Crohn’s disease, evaluating treatment efficacy, and conducting surveillance for dysplasia in longstanding IBD.
How does chromoendoscopy enhance IBD assessment?
Chromoendoscopy, an advanced endoscopic technique, utilizes dye-spray to enhance mucosal visualization. It significantly improves the detection of subtle mucosal abnormalities and dysplastic lesions, which is critical in managing longstanding IBD. This technique enables more targeted biopsies, leading to an increased yield of dysplasia detection compared to conventional white-light endoscopy.
What are the key endoscopic features of ulcerative colitis?
Ulcerative colitis is characterized by diffuse mucosal erythema, loss of vascular pattern, granularity, friability, and ulcerations. The disease typically presents with continuous and symmetrical involvement, starting from the rectum and extending proximally. In severe cases, pseudopolyps may be observed. The extent of mucosal involvement is directly correlated with disease severity, guiding therapeutic decision-making.
How does MR enterography contribute to IBD diagnosis?
MR enterography is a valuable imaging modality in IBD diagnosis, with a particular emphasis on Crohn’s disease. It provides high-resolution cross-sectional images of the small bowel without ionizing radiation exposure. MR enterography excels in detecting transmural inflammation, strictures, fistulae, and abscesses. Its superior soft tissue contrast allows for detailed evaluation of perianal disease and assessment of extraintestinal manifestations, making it an essential tool in the evaluation of IBD.
What are the current recommendations for dysplasia surveillance in IBD?
Current guidelines advocate for initiating dysplasia surveillance colonoscopies 8-10 years after disease onset for patients with extensive colitis. Surveillance intervals are stratified based on individual risk factors, disease duration, and previous findings. High-definition endoscopy with chromoendoscopy is preferred for optimal visualization. Targeted biopsies of suspicious lesions and random biopsies in each colonic segment are recommended. The aim is early detection of precancerous changes to prevent colorectal cancer development in IBD patients.
How effective is endoscopic balloon dilation for Crohn’s disease strictures?
Endoscopic balloon dilation is an effective minimally invasive treatment for short, fibrotic strictures in Crohn’s disease. Studies have shown technical success rates of 80-90% with clinical efficacy in 70-80% of cases. The procedure can provide symptomatic relief and potentially delay or avoid the need for surgical intervention. Patient selection, stricture characteristics, and post-procedure management are critical factors influencing outcomes.
What are the primary safety considerations for endoscopic procedures in IBD patients?
Key safety considerations for endoscopic procedures in IBD patients include:
1. Assessing disease activity and optimizing medical management pre-procedure.
2. Careful patient selection, particular for advanced therapeutic interventions.
3. Appropriate bowel preparation and management of medications (e.g., anticoagulants).
4. Vigilant monitoring during sedation, with a focus on patients with comorbidities.
5. Awareness of increased perforation risk in severely inflamed or fibrotic bowel segments.
6. Proper technique and equipment selection to minimize procedure-related complications.
7. Thorough post-procedure monitoring and patient education on possible adverse events.
How does fecal calprotectin contribute to IBD diagnosis and monitoring?
Fecal calprotectin is a highly sensitive biomarker of intestinal inflammation. It aids in differentiating between inflammatory and functional bowel disorders, reducing the need for unnecessary invasive procedures. For disease monitoring, fecal calprotectin levels correlate well with endoscopic disease activity, allowing for non-invasive assessment of mucosal healing and treatment response. Regular monitoring of fecal calprotectin can guide therapeutic decisions and predict relapse, enabling proactive management strategies in IBD care.
Source Links
- Diagnostic Procedures for Inflammatory Bowel Disease: Laboratory, Endoscopy, Pathology, Imaging, and Beyond – https://pmc.ncbi.nlm.nih.gov/articles/PMC11241288/
- Inflammatory bowel disease (IBD) – Diagnosis and treatment – https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/diagnosis-treatment/drc-20353320
- Best practices for using IBD endoscopic scoring systems – https://gastro.org/news/best-practices-for-using-ibd-endoscopic-scoring-systems/
- Laboratory Testing for the Diagnosis of Inflammatory Bowel Disease – https://www.myhealthtoolkit.com/web/public/brands/medicalpolicy/external-policies/laboratory-testing-for-the-diagnosis-of-inflammatory-bowel-disease/
- Role of Colonoscopy in Diagnosing Inflammatory Bowel Diseases – https://curasia.com/the-role-of-colonoscopy-in-diagnosing-inflammatory-bowel-diseases/
- Endoscopic diagnosis of inflammatory bowel disease in adults – https://www.uptodate.com/contents/endoscopic-diagnosis-of-inflammatory-bowel-disease-in-adults
- Testing and Diagnosis for Inflammatory Bowel Disease (IBD) – https://www.cdc.gov/inflammatory-bowel-disease/testing/index.html
- Endoscopic diagnosis and management of adult inflammatory bowel disease: a consensus document from the American Society for Gastrointestinal Endoscopy IBD Endoscopy Consensus Panel – PubMed – https://pubmed.ncbi.nlm.nih.gov/39425706/
- Artificial intelligence-enabled advanced endoscopic imaging to assess deep healing in inflammatory bowel disease – http://egastroenterology.bmj.com/content/2/3/e100090
- PDF – https://egastroenterology.bmj.com/content/egastro/2/3/e100090.full.pdf
- Automated Endoscopic Diagnosis in IBD: The Emerging Role of Artificial Intelligence – PubMed – https://pubmed.ncbi.nlm.nih.gov/39510689/
- AI for IBD: Will Emerging Technology Revolutionize Care? – https://www.gastroenterologyadvisor.com/features/ai-for-ibd/
- Advancing Colorectal Cancer Prevention in Inflammatory Bowel Disease (IBD): Challenges and Innovations in Endoscopic Surveillance – https://www.mdpi.com/2072-6694/17/1/60
- A Systematic Review and Meta-Analysis of Endoscopic Surveillance Studies for Detecting Dysplasia in Patients With Inflammatory Bowel Disease – PubMed – https://pubmed.ncbi.nlm.nih.gov/38738163
- Inflammatory Bowel Disease – IBD – https://arupconsult.com/content/inflammatory-bowel-disease
- Endoscopic Management of Strictures in Crohn’s Disease: An Unsolved Case – https://www.mdpi.com/2077-0383/13/16/4842
- No title found – https://www.e-ce.org/articles/search_result.php?term_type=keywords&term=Inflammatory bowel disease
- Crohn Disease – StatPearls – NCBI Bookshelf – https://www.ncbi.nlm.nih.gov/books/NBK436021/
- Inflammatory bowel disease (IBD) – https://www.beaconhealthsystem.org/library/diseases-and-conditions/inflammatory-bowel-disease-ibd?content_id=CON-20312396
- A Comprehensive Multidisciplinary Approach to Diagnosing Chronic Inflammatory Bowel Diseases: Integration of Clinical, Endoscopic, and Imaging Modalities – https://www.mdpi.com/2075-4418/14/14/1530