Key Takeaways
- Introduction to the Anatomy and Physiology of the Stomach
- Gross Anatomy of the Stomach: Structure and Regions
- Microscopic Anatomy: Layers and Cellular Composition
- Blood Supply and Innervation of the Stomach
The stomach is a vital muscular organ in the digestive system, responsible for breaking down food into nutrients. It combines mechanical and chemical processes to prepare meals for absorption in the intestines. This hollow structure stores, churns, and partially digests ingested material before passing it further.
Gastric functions rely on specialized regions, each contributing to digestion. Acid and enzymes dissolve food while protective mucus prevents self-damage. Understanding these mechanisms helps diagnose disorders like ulcers or gastritis.
Key Takeaways
- The stomach mechanically churns and chemically breaks down food.
- It secretes acids and enzymes for digestion.
- Mucosal layers protect against self-digestion.
- Different regions have unique roles in processing meals.
- Knowledge of gastric structure aids in diagnosing disorders.
Introduction to the Anatomy and Physiology of the Stomach
Measuring roughly the size of a fist when empty, this muscular organ can expand to hold up to four liters of content. The stomach is located in the upper abdomen, nestled between the esophagus and duodenum. Its flexible structure allows temporary food storage before gradual release into the small intestine.
Digestion follows a three-phase process: cephalic (anticipatory), gastric (mechanical mixing), and intestinal (controlled emptying). Vagus nerve signals coordinate these stages, linking brain activity to gastric functions.
While most nutrient absorption occurs downstream, the stomach absorbs small molecules like alcohol and water. Distension of its walls triggers hunger signals, creating feedback loops with the brain.
“Gastric motility and secretion are finely tuned by autonomic regulation, ensuring efficient digestion.”
This organ’s ability to churn and acidify food underscores its role as a digestive workhorse. Protective mucus shields its lining from corrosive juices, balancing aggressive and defensive mechanisms.
Gross Anatomy of the Stomach: Structure and Regions
Four primary regions define the stomach’s architecture, facilitating mechanical and chemical breakdown. Each part stomach contributes uniquely to digestion, from temporary storage to controlled emptying. Structural variations reflect functional specialization, ensuring efficient nutrient processing.
The Four Main Regions
The cardia encircles the esophageal opening, preventing acid reflux. Above it, the dome-shaped fundus stores undigested food and gases. The central body mixes contents with gastric juices, while the funnel-shaped pylorus regulates passage into the duodenum.
Curvatures and Their Significance
The lesser curvature forms a concave border, measuring 10cm, while the convex greater curvature spans 40cm. Vascular networks along these curves influence surgical approaches. Histological transitions near the cardia mark shifts from esophageal to gastric epithelium.
Pyloric Sphincter Mechanics
A 1cm-thick muscular ring, the pyloric sphincter, maintains 15–30mmHg pressure to prevent backflow. Its 2.5cm canal ensures gradual chyme release. Radiographic studies highlight this landmark during diagnostic imaging.
“The pyloric sphincter’s dynamic pressure adjustments are critical for preventing duodenal ulceration.”
Functional differentiation between regions—gas storage in the fundus versus mixing in the body—underscores the stomach’s compartmentalized design. This structural precision supports its role as a digestive linchpin.
Microscopic Anatomy: Layers and Cellular Composition
Histological examination uncovers four distinct layers that enable gastric functions. From innermost to outermost, these include the mucosa, submucosa, muscularis externa, and serosa. Each contributes uniquely to digestion and structural integrity.
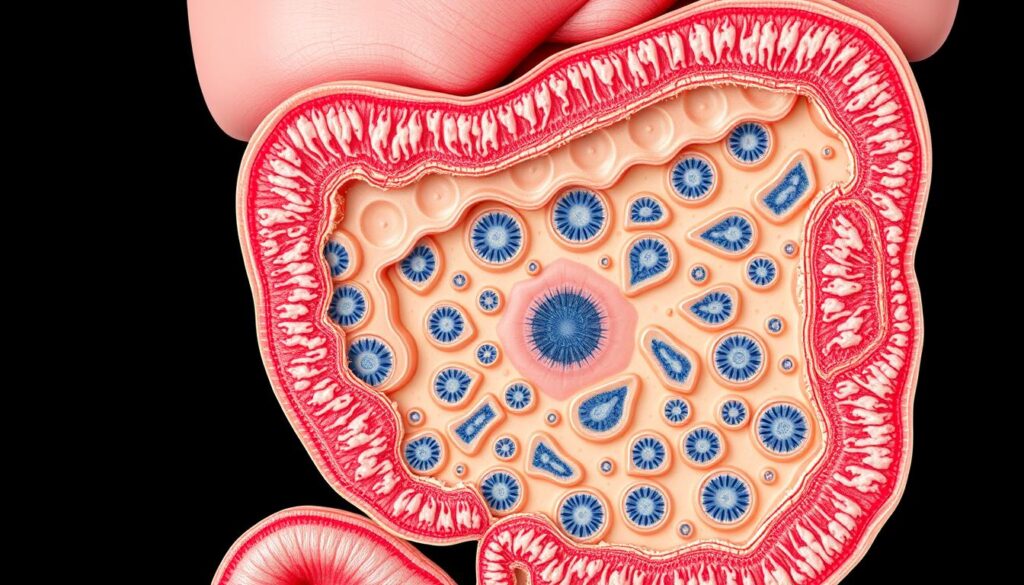
Mucosa, Submucosa, Muscularis Externa, and Serosa
The mucosa features columnar epithelium, renewing completely every 3–6 days. Its surface folds increase contact with food. Beneath lies the submucosa, a vascular connective tissue layer supplying nutrients.
The muscularis externa contains oblique, circular, and longitudinal muscle layers. These orchestrate churning motions. Outermost, the serosa provides a protective visceral peritoneal coating.
Gastric Glands and Their Secretory Cells
Specialized cells populate gastric glands. Key types include:
| Cell Type | Secretions | Function |
|---|---|---|
| Parietal | HCl, intrinsic factor | Acidifies lumen; aids B12 absorption |
| Chief | Pepsinogen | Protein digestion |
| Mucous neck | Alkaline mucus | Protects against acid |
“Parietal cells generate 2L of HCl daily via H+/K+ ATPase pumps—a proton exchange critical for digestion.”
Role of Mucus and the Mucosal Barrier
Surface mucous cells secrete bicarbonate-rich mucus, maintaining a pH 7 epithelial surface despite luminal pH 1.5–2. Tight junctions with claudins/occludins prevent acid leakage.
This barrier prevents autodigestion while permitting nutrient processing—a balance essential for gastric health.
Blood Supply and Innervation of the Stomach
Optimal gastric function depends on robust vascular networks and precise neural control. These systems ensure oxygen delivery, waste removal, and coordinated motility. Disruptions in either component may impair digestion or increase ulcer risks.
Arterial Supply: Gastric and Gastroomental Arteries
The celiac trunk branches into three key arteries: left gastric, splenic, and common hepatic. The left gastric artery supplies the lesser curvature, while the right gastric artery (from the hepatic artery) forms anastomoses. Gastroomental arteries follow the greater curvature, with Barkow’s arcade providing collateral circulation during partial gastrectomies.
Venous Drainage and Lymphatic System
Venous blood flows into the portal system via coronary and splenic veins. This route directs nutrients to the liver for processing. Lymphatic drainage follows perigastric and celiac nodes, critical for oncological staging. Watershed areas near the fundus are vulnerable to ischemia.
Parasympathetic and Sympathetic Innervation
The vagus nerve delivers parasympathetic fibers, enhancing secretion and motility. Anterior (Latarjet) and posterior trunks branch extensively. Sympathetic fibers from T6–T9 inhibit motility via the celiac plexus. Neurotransmitters like VIP and nitric oxide mediate relaxation.
“Vagal innervation accounts for 90% of gastric neural input, underscoring its dominance in digestive regulation.”
- Surgical note: Barkow’s arcade preserves blood flow during resection.
- Clinical insight: Lymph node metastasis patterns guide cancer treatment.
- Functional impact: Autonomic imbalances contribute to gastroparesis.
Mechanical Digestion: How the Stomach Churns and Mixes Food
Mechanical digestion transforms solid meals into semi-liquid chyme through coordinated muscular activity. This process relies on specialized contractions that break food while mixing it with gastric juices. Three cycles per minute ensure thorough homogenization of contents.
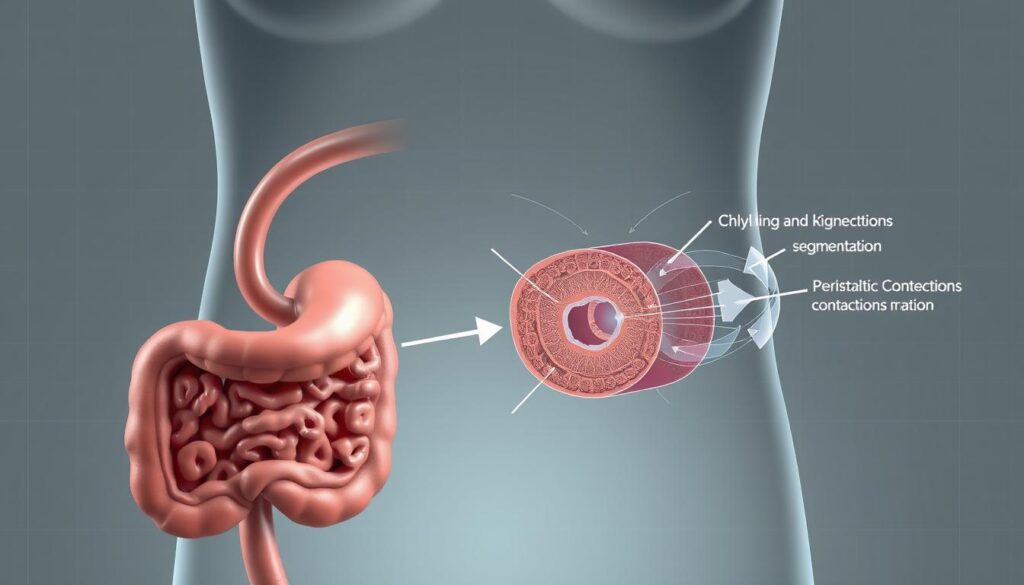
Mixing Waves and Gastric Motility
Electrical slow waves originate in pacemaker cells at 3 cycles/minute. These depolarizations trigger peristaltic movements propagating from the fundus. Antral systole generates 50-70cm H2O pressure, pulverizing solids.
Segmental contractions create localized mixing zones. Vagovagal reflexes adjust motility based on meal volume. Manometric studies reveal disrupted patterns in gastroparesis patients.
The Role of the Muscularis Externa
Three muscle layers enable multidirectional churning:
- Oblique fibers enhance fundic expansion
- Circular muscles propel contents distally
- Longitudinal fibers shorten the organ
This arrangement creates a mechanical digestion gradient. The pylorus acts as a sieve, permitting only particles under 2mm to pass.
“Gastric accommodation involves receptive relaxation mediated by nitric oxide, allowing volume increases without pressure spikes.”
Rheological changes during chyme formation optimize nutrient exposure. The muscle coordination ensures efficient processing while preventing premature emptying.
Chemical Digestion: Gastric Secretions and Enzymes
Chemical digestion transforms food through powerful secretions and specialized enzymes. This process relies on precise coordination between cells, pH levels, and hormonal signals. Disruptions in these mechanisms impair nutrient breakdown and increase disease risks.
Hydrochloric Acid and Pepsinogen Activation
Parietal cells produce hydrochloric acid at 160mmol/L concentrations—enough to dissolve metal. Carbonic anhydrase converts CO2 and H2O into bicarbonate and protons, fueling proton pumps. The resulting pH
- Denatures proteins
- Activates pepsinogen into pepsin
- Kills ingested pathogens
Chief cells release inactive pepsinogen, which self-cleaves at low pH. This proteolytic cascade amplifies protein digestion efficiency.
“Histamine from enterochromaffin-like cells potentiates acid secretion via H2 receptors—a target for ulcer medications.”
Digestive Hormones: Gastrin, Ghrelin, and Somatostatin
Gastrin-17 (half-life: 5 minutes) stimulates acid release when food enters the antrum. Ghrelin increases appetite, while somatostatin inhibits both hormones. Key interactions include:
- Gastric secretion surges during meals
- Negative feedback prevents mucosal damage
- Phase-specific therapies (PPIs vs H2 blockers)
The Cephalic, Gastric, and Intestinal Phases of Secretion
Digestive phases refine gastric secretion timing:
- Cephalic: Vagus nerve primes enzymes via sight/smell
- Gastric: Distension and peptides trigger local reflexes
- Intestinal: Duodenal hormones slow emptying
This tiered regulation ensures optimal nutrient processing while protecting tissues.
The Stomach’s Role in Nutrient Absorption and Protection
Beyond digestion, this organ plays a critical role in selective nutrient absorption and self-protection. Its mucosal lining facilitates limited molecular uptake while defending against corrosive juices. This dual process ensures efficient nutrient processing without tissue damage.
Limited Absorption: Alcohol, Water, and Medications
The stomach absorbs 20% of ethanol directly—faster than intestinal uptake due to vascularization. Water crosses the epithelium via osmosis, while certain medications like aspirin exploit gastric pH for absorption.
First-pass metabolism occurs when drugs enter the portal circulation post-absorption. This impacts bioavailability, as seen with nitroglycerin’s 90% hepatic extraction. Key factors influencing uptake:
- Lipid solubility enhances diffusion
- Ionized molecules resist absorption
- Gastric emptying rate alters exposure time
How the Stomach Prevents Self-Digestion
A dynamic mucosal barrier safeguards epithelial cells. Surface mucous cells secrete 5mmol/hr bicarbonate, neutralizing acid near the lining. Tight junctions with claudin-18 proteins restrict proton leakage.
Prostaglandin E2 maintains mucosal integrity by:
- Stimulating mucus production
- Enhancing blood flow
- Activating cellular repair
“Epithelial restitution occurs within 15 minutes post-injury, showcasing the stomach’s remarkable regenerative capacity.”
Reactive oxygen species are neutralized by glutathione peroxidase. This multi-layered defense ensures continuous function despite harsh luminal conditions.
Clinical Insights: Common Stomach Disorders
Gastric disorders affect millions globally, with varying degrees of severity and clinical presentations. These conditions often stem from imbalances between protective mechanisms and aggressive factors like acid secretion. Early recognition of symptoms enables timely intervention to prevent complications.
Peptic Ulcers and Helicobacter pylori
Approximately 50% of the global population harbors Helicobacter pylori, with 15% developing ulcers. This gram-negative bacterium damages the mucosa through specific virulence factors:
| Factor | Mechanism | Clinical Impact |
|---|---|---|
| CagA | Disrupts cell signaling | Promotes carcinogenesis |
| VacA | Creates vacuoles in epithelium | Increases ulcer risk |
Patients typically report burning epigastric pain that improves with food. The updated Sydney system guides histological grading of mucosal damage during endoscopic evaluation.
“H. pylori eradication therapy reduces ulcer recurrence rates by 80% when combined with proton pump inhibitors.”
Hiatal Hernias: Causes and Symptoms
Type I-IV hiatal hernias occur when gastric portions protrude through the diaphragmatic hiatus. Sliding (Type I) hernias account for 95% of cases, while paraesophageal types carry higher strangulation risks.
Common symptoms include:
- Heartburn exacerbated by bending
- Regurgitation of acidic contents
- Chest pain mimicking cardiac issues
The Siewert classification further categorizes gastroesophageal junction tumors associated with chronic herniation.
Gastritis and Gastric Cancer
Chronic inflammation progresses through defined stages:
- Superficial gastritis (reversible)
- Atrophic changes with metaplasia
- Dysplasia per Houston protocol criteria
The endoscopic Kyoto classification identifies high-risk patterns for malignancy. Regular surveillance is critical for patients with:
- Intestinal metaplasia
- Family history of gastric cancer
- Persistent H. pylori infection
Early gastric cancers often present with nonspecific symptoms, underscoring the importance of risk stratification and screening in high-prevalence regions.
Conclusion: The Stomach’s Vital Role in Digestion and Health
As a key component of the digestive system, this organ orchestrates complex processes essential for nutrient breakdown. Its dual mechanical-chemical function ensures efficient digestion while protecting mucosal integrity.
Emerging research explores gut-brain axis interactions and microbial influences on gastric health. Clinical studies link anatomical variants to disorders like gastroparesis or metaplasia progression.
Preventive strategies emphasize dietary modifications and early H. pylori eradication. Multidisciplinary care combines gastroenterology, nutrition, and surgery for complex cases.
FAQ
What are the main regions of the stomach?
The stomach is divided into four primary regions: the cardia, fundus, body, and pylorus. Each plays a distinct role in digestion and gastric secretion.
How does the pyloric sphincter function?
The pyloric sphincter regulates the passage of partially digested food from the stomach into the duodenum. It prevents backflow and ensures controlled release.
What cells produce stomach acid?
Parietal cells in gastric glands secrete hydrochloric acid, which aids in protein digestion and activates pepsinogen into pepsin.
What protects the stomach from self-digestion?
A thick mucus layer and bicarbonate secretion form the mucosal barrier, shielding the stomach lining from corrosive acid and enzymes.
How does the stomach mechanically break down food?
The muscularis externa generates mixing waves, churning food into chyme through rhythmic contractions.
What hormones regulate gastric secretion?
Gastrin stimulates acid production, while somatostatin inhibits it. Ghrelin signals hunger to the brain.
Can the stomach absorb nutrients?
Limited absorption occurs, primarily for water, alcohol, and certain medications. Most nutrients are absorbed in the small intestine.
What causes peptic ulcers?
Helicobacter pylori infection or prolonged NSAID use erodes the mucosal barrier, allowing acid to damage the stomach lining.
How does gastritis develop?
Inflammation of the gastric mucosa results from infections, autoimmune reactions, or irritants like alcohol and bile reflux.